Virtual Doctor: How Online Medical Consultations Are Changing Healthcare The healthcare field is undergoing a significant revolution with technology helping in closing the gap between the patient and the healthcare provider. The emergence of virtual healthcare services could be described as one of the most influential ones since it enables individuals to obtain medical care without going to a clinic or a hospital. In terms of treating minor ailments to follow-ups, digital healthcare is transforming the issue of convenience, access, and care continuity. Due to the popularization of internet connectivity and smart devices, virtual consultations are no longer a temporary solution, but a lasting change in today’s healthcare provision. What Is Virtual Doctor? A virtual doctor is a qualified health practitioner who offers medical care opportunities through the online platform. In Online doctor consultation, patients are able to meet with physicians through video calls, audio calls or secure messaging. This model removes the geographical limits and allows medical consultation within a short time without travel. A Virtual doctor consultation is similar to that of a real-life visit with patients being given an opportunity to describe the symptoms, provide a medical history and given guidance, prescription and/or referral where applicable. The Way Virtual Doctor Services Work? The method of reaching virtual healthcare is supposed to be easy and convenient. Patients would usually enrol on a platform, select a doctor, book or start a session. The overall workflow entails: Establishing a safe profile in a medical site. Choosing the form of consultation needed. Posting of past health history where necessary. Communicating with a physician chat or video. Giving instructions or advice, following the instructions or advice, prescription. Most individuals would now rather talk to a doctor online since it is both time saving and it eliminates the waiting rooms, particularly when there is no emergency. The Advantages of a Virtual Doctor There are a number of benefits of virtual healthcare to the patients, caregivers, and even care systems. Key benefits include: Easy access to health care counsel. Decreased travel and waiting time. Better access by rural or mobility impaired patients. Cost-effective consultations Enhanced continuity of care Online medical consultation can be especially useful to people with chronic illnesses that need regular check-ups but do not need to visit the clinic often. Diseases that Virtual Doctors Treat E-doctors are prepared to deal with the most diverse number of non-emergency cases. Although it is not applicable in every circumstance, numerous health-related issues can be solved online. The most typical types of conditions are: Cold, influenza, seasonal infections. Allergies and minor respiratory problems. Skin conditions e.g. rashes or acne. Digestive problems Mental illnesses such as anxiety and stress. Refill of medicines and follow ups. The Telemedicine doctor can also advise the patients on whether they need a face-to-face consultation or not to provide them with safe and proper treatment. Virtual Doctor Vs In-Clinic Visit Although both of them are useful options, the virtual and in-clinic visits differ in the areas of their application and scope. Virtual consultations are suitable in case of: Non-urgent medical issues Follow-up appointments General health advice Second opinions In-clinic visits will always be necessary in: Physical examinations Laboratory or radiographic testing. Surgical procedures Emergency care Virtual care is the complement of traditional care, which does not and cannot substitute it to a hybrid model that benefits patients. Book Your Free Marketing Consultation Virtual Doctor Services Technology Virtual healthcare depends on a high-grade digital infrastructure to work effectively. Safe services guarantee the secrecy of patients and provide smooth communication. Core technologies include: Video and audio communication are encrypted. Implementation of electronic health records. AI-assisted symptom assessment instruments. Cloud-based data storage Video doctor consultation provides the opportunity to interact in real-time, which allows doctors to receive an image of some symptoms, and develop an atmosphere of communication with the patient just as it would be during a face-to-face meeting. Who makes use of Virtual Doctor Services? The virtual healthcare can also be received by a great number of people, as long as they have access to the internet and a compatible device. It is especially useful for: Busy professionals Older patients who are mobility impaired. Residents of remote places. Parents who need hasty tips on children. Medical tourists seeking advice. A Virtual doctor appointment system is currently available on many platforms that can fit other schedules and time zones. In some areas, where healthcare is scarce like in South Asia, an online doctor in Pakistan has been adopted as a viable option in achieving medical care in time. Disadvantages of the Virtual Doctor Consultations Even though virtual healthcare has several benefits, it has some shortcomings that patients need to know. Key challenges include: The inability to carry out physical exams. Relying on patient-reported symptoms. Poor emergency capability. Technical problems like ineffective connectivity. A 24/7 online doctor service is better but by no means the alternative to the emergency medical care in the critical cases. Future of Virtual Doctors Virtual healthcare has a bright future due to the fact that technology keeps on advancing. It is assumed that artificial intelligence, wearable devices, and remote monitoring tools may improve the accuracy and personalized care. The future developments might involve: Wearable real-time health data integration. Greater coverage of expert services. Better AI-based decision support. Wide virtual visit insurance. Remote doctor consultation will more and more depend on digital biomarkers and data provided by patients to clinically act. Some Advice on a Successful Virtual Doctor Consultation The most out of a virtual visit will be preparedness. Helpful tips include: Make sure the internet is not going dead. Select a comfortable place that is bright. Make a list of questions and symptoms. Prepare medical records and medications. Speak candidly and vividly describe. Online specialist consultation is more efficient in case patients express themselves effectively and adhere to medical recommendations. Conclusion Virtual doctor services are transforming the healthcare sector by facilitating accessibility, efficiency and patient-centred medical advice. On the one hand, Online GP consultation are not a substitute
How to Secure Patient Data from Ransomware? The advent of the era of technology in the healthcare sector has made it more vital now than ever to protect patient data from ransomware. Healthcare organizations are a key target for cyber attackers because they hold vast quantities of sensitive personal and health information. The impact of a ransomware attack can be financial loss, damage to reputation, HIPAA breaches, and most significantly, disruption of essential patient care. In this guide, we cover the nature of ransomware, why patient data is an attractive target, and how to have effective ransomware protection strategies in place to protect your systems and ensure healthcare cybersecurity. What Is Ransomware? Ransomware is malware that encrypts data and systems, holding the users at ransom until payment is received. Such attacks often begin with a phishing email, suspicious attachment, or exploit on old software. Ransomware in healthcare, minutes of downtime can result in loss of life, so organizations will pay. Types of Ransomware There are many different types of ransomware: Crypto Ransomware: It encrypts important data, making it unreadable unless a decryption key is generated. Locker Ransomware: It locks down the whole device , with the only exception being application and file access. Double Extortion Ransomware: It encrypts data and additionally exfiltrates it. Threat actors threaten to pay or publish stolen data, doubling the pressure on victims. Current Healthcare Ransomware Trends The healthcare industry remains under siege: Clinics and hospitals are being targeted with an overwhelming increase in targeted attacks, where most prefer to close emergency rooms. Phishing methods are becoming complex with AI usage. Remote desktop protocols (RDP) are being targeted heavily. Third-party vendors and their connected devices are currently the best attack surfaces. Why Patient Data Is So Valuable? High Market Value of Medical Records Medical records differ from credit card information since they hold fixed details: names, dates of birth, insurance policy numbers, and complex medical history. Due to this, they are worth a lot of money on the dark web, going for 10–20 times more money than other personal data. Exploitation of Stolen Information Cybercriminals use medical information in various ways: Insurance fraud: Filing incorrect claims based on stolen insurance information. Identity theft: Opening unauthorized accounts or seeking medical treatment based on data. Misuse of prescriptions: Acquiring drugs or controlled substances illegally. Consequences of a Violation of Healthcare Information Violation of healthcare information can have serious repercussions: HIPAA violation: Heavy penalties from regulating authorities. Legal proceeding: Class action lawsuits by harmed patients. Federal investigations: Leading to operational audits and loss of licenses. Impact on Clinical and Operations Ransomware cyberattacks induce system downtime that slows down diagnoses and treatments, with the risk of jeopardizing patient outcomes. Patients also lose confidence in healthcare organizations that fail to keep secure medical records. Top Tactics to Safeguard Patient Data Adopt a Cybersecurity Framework Formulate an overall plan incorporating: Risk assessments to define vulnerabilities. Well-articulated cybersecurity policies and governance. Cybersecurity guidance from consultants. Strengthen Access Control Mechanisms Adopt strong access control by: Adopting role-based access to limit unwanted exposure. Activated multi-factor authentication (MFA). Monitoring login activity and system use for anomalies. Keep Software Current Software updates minimize the risk of exploits: Patch serious software vulnerabilities in a timely fashion. Utilize up-to-date antivirus and endpoint protection software. Scan legacy systems for hardening or retirement. Implement a Zero Trust Policy Trust no system or user: Verify all access requests. Enforce least-privilege rules. Randomly monitor user activity on the network. Vendor Risk Management Vendors and third-party service providers share the same patient data security needs: Screen vendors based on cybersecurity best practices for clinics. Place cybersecurity terms in contracts. Audit their access to sensitive patient information. Book Free Demo Different Data Protection Techniques Encrypt Patient Information Encrypting patient data ensures that even if the data is stolen, it is not usable: Use an industry standard such as AES-256. Encrypt data in transit and at rest. Use encryption for backup, email, and portable devices. Backup and Disaster Recovery Good backup practice lessens the impact of attacks: Adopt 3-2-1 rule (three copies, two different types of storage, one offsite). Regularly test backup integrity. Maintain backups on offline or immutable storage platforms. Secure EMR Systems EMR data security is commonly targeted: Select EMR systems with inherent security features. Enable audit trails and access logging. Integrate EMRs into overall cybersecurity efforts. Cloud Security for Healthcare Cloud security for healthcare providers is frequently utilized for storage and operations: Partner with HIPAA-approved cloud vendors. Employ end-to-end encryption of data stored in the cloud. Audit access and configuration options regularly. Physical Security Controls Physical security is frequently neglected: Restrict data center access via biometric or keycard authentication. Perform surveillance and regular inspections. Lock down devices in patient areas and take unattended devices away. Endpoint Detection and Response (EDR) EDR tools assist in detecting and quarantining ransomware attacks: Automatically monitor behaviors and detect suspicious activity. Quarantine infected systems from the network.
Ethics of AI in Healthcare Artificial Intelligence (AI) is revolutionizing the healthcare sector with advancements in diagnostics, treatment planning, predictive analysis, and administrative effectiveness. Right from AI-enabled radiology to virtual health assistants, applications of intelligent systems are enabling doctors to render faster, more precise, and more customized care. Yet, these advantages are paired with stern moral issues. AI algorithmic discrimination, patient self-determination, patient data privacy, AI accountability, and transparency are some of the direct concerns. Healthcare AI ethics is not an add-on; it is an urgent framework demanded to inform responsible innovation. This blog acknowledges the AI bias in medicine and highlights significant ethical standards and best practices required for ethical use and deployment. The Role of AI in Healthcare The uses of AI in the healthcare sector are far-reaching and continuously changing. Here are some of the main areas where AI is making its mark, with potential and moral issues. 1. Diagnostic Imaging AI algorithms analyze X-rays, MRIs, and CT scans quickly than human radiologists. AI speeds up early disease diagnosis like cancer, stroke, and retinal diseases. This improves diagnostic accuracy and speed, yet bias in AI analysis is a problem if the training data are not representative and ends in misdiagnosis of minority populations. 2. Predictive Analytics Machine learning algorithms can predict patient decline, readmission to the hospital, or outbreak of epidemics. These systems enhance preventative treatment but can develop responsibility issues in AI systems when the prediction is wrong or induces unwarranted panic. 3. Personalized treatment AI can provide personalized treatment regimens based on patient history and international medical literature. These applications are excellent decision tools, but still require human supervision in AI-enhanced care. An entirely automated process risks dehumanizing care and reducing clinician autonomy. 4. Virtual Health Assistants Chatbots and virtual assistants enable activities such as scheduling appointments, symptom checking, and medication reminders. These are fashionable but raise ethical concerns in AI diagnostics and data security in AI healthcare tools. 5. Administrative Automation Paper is minimized to an absolute minimum, and billing, insurance processing, and record-keeping are accelerated through AI. Although it streamlines procedures, automated errors or biases can be disastrous, particularly for insurance claims and medical coding. Ethical AI Practice in Medicine Ethical AI practice in medicine relies on integrating novel technologies into fundamental values of medical ethics and artificial intelligence, beneficence, non-maleficence, justice, autonomy, and accountability in AI systems. 1. Beneficence and Non-Maleficence AI technologies must be designed to benefit patient health without harming them. Algorithms must be carefully examined for accuracy, safety, and representativeness. Failing to correct AI errors or admitting poorly trained models to practice contravenes this value. 2. Autonomy and Informed Consent Patients should be informed whenever AI is applied in their care and be capable of comprehending its use. Ethical AI must ensure informed consent and AI-informed care. This is achieved by providing transparent descriptions of how AI affects diagnoses or choices, possible harm, and information on what data is gathered. 3. Fairness and Justice There is fairness in healthcare AI algorithms in the sense of treating all patients equally, regardless of race, gender, or socioeconomic status. AI algorithms created from biased data may further aggravate existing biases. Algorithms have to be tested on heterogeneous populations by developers. 4. Transparency and Explainability One of the most controversial issues is the “black box” nature of AI. Clinicians and patients require transparency in medical AI so that they can trust its recommendations. Explainable AI (XAI) can enhance understanding and responsibility by demonstrating the mechanism by whereby conclusions were drawn. 5. Responsibility and Liability In medicine, if something goes wrong, there has to be clear delegation of responsibility. If a computer AI is giving a false diagnosis or advice, is the doctor, the hospital, or the programmer at fault? There has to be legal and ethical responsibility assigned to AI systems. 6. Privacy and Confidentiality Artificial intelligence systems need large quantities of health information, typically drawn from electronic health records (EHRs), imaging data, wearables, or mobile apps. Preserving data privacy in AI systems involves protecting consent, de-identifying data, and complying with policies such as HIPAA and GDPR. Greatest Challenges to Ethical Adoption of AI Despite the best efforts globally towards the ethical implications of AI in healthcare, some challenges are responsible for slowing it down: 1. Biased Training Data If AI models are trained mainly on information about specific geographic or demographic populations, what emerges won’t apply to others. This creates AI bias in healthcare, which exacerbates health disparities rather than enhancing results. 2. Flawed Regulation AI development is outpacing regulation. In many regions, there are no clear standards for clinical validation, deployment, or post-market surveillance of AI tools. As a result, developers may not be held accountable for flaws or misuse. 3. Lack of Explainability Deep learning models are often complex and difficult to interpret. If clinicians cannot understand or challenge an AI’s output, ethical problems arise, particularly in life-or-death scenarios where reasoning must be transparent. 4. Inconsistent Human-AI Collaboration AI must be employed to augment, not substitute for, healthcare professionals. But if not taught to engage with AI systems, clinicians will be likely to rely too heavily on buggy suggestions or ignore rich information. Managing human supervision of AI-driven care is crucial. Book Free Demo Best Practices for Ethical AI in Healthcare Software developers and healthcare providers should incorporate practices to maximize the application of AI for good and patient-oriented purposes. 1. Use Varied, Representative Data Training data must cover all ethnic backgrounds, ages, sexes, and histories to prevent AI diagnosis bias. Algorithmic bias can be identified and rectified over time through ongoing audits. 2. Use Explainable AI Use transparent and explainable models that offer justification for their suggestions to establish trust among healthcare providers and patients and enable AI decision-making in clinical settings based on informed information. 3. Design Oversight Mechanisms Hospitals and clinics should establish AI ethics committees that include a balance of ethicists, clinicians, patients, and data scientists as members. These committees can pre-screen tools before deployment
AI in Telehealth: Transforming Virtual Care with Smart Technology With digital health taking off around the globe, Artificial intelligence in healthcare is introducing a new paradigm of customized, effective, and affordable virtual care. Telehealth, once a novelty relegated to rural or underserved locations, has now transformed into a mainstream healthcare practice, particularly during the COVID-19 pandemic era. AI has driven this growth much faster through automating workflows, improving decision-making, and supporting more preventative models of care. From Telemedicine AI tools that support physicians with diagnoses to AI-based healthcare apps empowering patients to manage chronic illnesses, artificial intelligence is transforming how care is delivered remotely. With the promise of cost savings, scalability, and better patient outcomes, AI is no longer something out of the future it is the future and present of telehealth. The Evolution of Telehealth Telehealth has existed for decades, with initial simple audio and video interactions between patients and physicians. As technology evolved with better internet connectivity, wearable devices, and cloud computing, the reach and availability of virtual medical services improved. However, a complete shift only occurred with the injection of AI technologies. The incorporation of Machine learning in telehealth enables systems to learn from patient information and get better with time, which helps providers deliver more accurate and effective care. The transition towards telehealth automation is also minimizing administrative weight, simplifying workflows for patients, and enabling healthcare professionals to concentrate more on important tasks Telehealth is not just video calls anymore. It now involves remote patient monitoring with AI, mobile health apps, and even AI-driven robots that engage patients. The convergence of telehealth and AI provides a more complete, interactive, and data-based solution for healthcare. Key Applications of AI in Telehealth AI-Based Diagnostics: One of the most compelling uses of AI in telemedicine is in AI-based healthcare apps diagnostics. Through patient history, lab tests, and image analysis, AI can assist clinicians in achieving faster and more accurate diagnoses. This reduces diagnostic error and reduces treatment time both essential in managing health outcomes. AI for Virtual Consultations: Virtual consultation AI leverages natural language processing (NLP) and machine learning to allow real-time doctor-patient interaction. Conversational speech may be transcribed by AI systems, provide possible diagnoses, or even alert providers to inconsistencies or left-out information within a patient’s clinical history. AI for Patient Triage: In crises or peak-demand cases, AI patient triage prioritizes cases according to severity. AI programs examine symptoms and medical histories to direct patients to the right level of care, self-care, virtual consultation, or emergency care. Remote Patient Monitoring: With the advent of wearables and IoT devices, remote patient monitoring using AI has also picked up much steam. Data from heart rate monitors, glucose meters, and other sensors is interpreted by AI algorithms to identify abnormalities and alert doctors in real time. Predictive Analytics in Telemedicine: Predictive analytics for telemedicine helps healthcare professionals anticipate complications even before they occur. AI can recognize trends and patterns in patient information to predict hospital readmissions, medication non-adherence, or impending disease outbreaks. Chronic Disease Management: For patients suffering from chronic diseases, AI chronic disease management offers sustained, individualized care. AI algorithms can observe vitals, modify treatment suggestions, and warn healthcare professionals about deteriorating conditions, allowing for more proactive intervention. Benefits of AI-Enhanced Telehealth Enhanced Accuracy and Efficiency: AI technologies automate processes involving the execution of routine tasks and enable informed decisions. Healthcare providers are given tools that learn and improve continuously in AI-based diagnostics and machine learning, which in turn leads to higher clinical accuracy. Increased Accessibility: By triaging and consultative services using AI, healthcare services are made more available through rural or underserved areas. 24/7 access to health care is offered by the Chatbots in telehealth and the AI-based virtual consultations, especially to people who have a limited mobility or no access to traditional clinics. Personalized Patient Care: AI analyzes overwhelming volumes of patient information in order to produce highly individualized recommendations. Healthcare apps based on AI can be adjusted to the peculiarities of each patient, making fitness, nutrition, and medication plans tailored to meet specific needs; this will increase engagement and outcomes. Cost Savings: AI automation lessens the necessity for in-office visits and eliminates excessive tests or procedures. Telehealth automation slashes administrative and operational expenses considerably, rendering healthcare more affordable. Early Detection and Prevention: With predictive analytics in telemedicine, possible health threats can be identified early. AI algorithms evaluate past and present data to raise warning flags about chronic conditions or acute illnesses, often before symptoms become apparent. Less Burnout for Clinicians: By handling routine questions, bureaucratic paperwork, and data entry, AI lets clinicians off bureaucratic duties. This enables them to focus on more relevant cases, therefore improving their job satisfaction and preventing burnout. Book Free Demo The Future of AI in Virtual Healthcare The prospects for AI in telehealth are huge. Advances in healthcare, Natural language processing in healthcare will make patients’ interactions with AI systems less formal and more sensible. NLP can not only be utilized to record consultations but also to monitor patient sentiment, mood, and mental health status. Another critical growth space is AI-powered healthcare applications, which will become smarter and more user-focused. Such applications will harness behavioral information and feedback to improve and evolve continuously, making health plans seamless. Telemedicine AI systems will continue to develop, whereby they will be multi-modal systems for diagnostics, treatment planning, and follow-up management. Interoperability will improve as AI systems will be able to draw and work with data from various e-health records, lab systems, and patient-generated sources. Conclusion The rollout of artificial intelligence throughout healthcare is revolutionizing the telehealth by facilitating more intelligent, faster, and personalized virtual care. From remote patient monitoring with help of AI to predictive analytics for telemedicine, AI is changing all patient touchpoints. Looking forward, the collaboration between clinicians, technologists, and policymakers will be important in actualising the full potential of AI in telehealth. Smart
How to Get More Repeat Bookings with Clinic Management Software? In today’s competitive healthcare environment, private clinics and practices have to not only gain new clients but also retain established ones. Boosting the patient return rate through repeat bookings is one of the core elements of maintaining patients and running a sustainable, long-term business. The modern clinic software can be one of the most potent ways to provoke this. With integrated functionalities like auto-reminders, communication management, and follow-up scheduling, it ensures ease-to-access communication for healthcare professionals while keeping their operations lean. Understanding Repeat Bookings Repeat bookings mean the patients visiting a clinic for a Follow-up appointment system, continued treatment, or prevention. It is a sign of trust, satisfaction on the part of the patient, and an eventual continuation of the patient-clinician relationship. It ensures consistent revenue for the practice and aids in enhancing the health outcome of the patient due to continuity of care. Why Repeat Booking Matters? Follow-up patients are easier to get through the treatment protocol, are good referral sources, and spread the word about your practice. They are also cheaper to keep than to acquire, hence they are vital organs for the success and well-being of any medical cash flow. Therefore, clinics must maintain a balance between maintaining existing patients and attracting new ones. Moreover, frequent patient visits allow healthcare providers to deliver better personalized care and track progress effectively. In the long run, this increases trust and contributes to better community health outcomes. Common Barriers to Repeat Bookings Before diving into how to enhance repeat bookings, it’s important to identify what might prevent them: Long waiting times Poor follow-up communication Forgetting appointments Inconvenient scheduling process Lack of engagement or motivation These are challenges that have a negative impact on patient experience in clinics and result in lost opportunities for follow-up treatment. Book Free Demo Key Features in Clinic Management Software That Drive Repeat Bookings Current clinic management software advantages go well beyond the convenience of administrative tasks. They encompass dedicated tools that directly affect repeat bookings: Online Appointment Scheduling: Patients appreciate Online appointment scheduling for clinics. A system that provides online appointment booking for clinics enables patients to schedule follow-ups at any time, from anywhere. This self-service option is particularly appealing to younger, technology-savvy patients. Automated Reminders: No-shows are frequent, but usually accidental. With appointment reminder software for physicians, repeat bookings through automated SMS, email, or app reminders can minimize no-shows and prompt early bookings. Built-in Communication Tools: Successful follow-up will frequently rest upon continuous communication. EMR with built-in communication tools allow clinicians to deliver updates, lab results, and reminders—all patient-keeping opportunities. Scheduling for Follow-up and Recall: Staff can be reminded by clinic software or even auto-schedule the next appointment using diagnosis or treatment plans to keep a solid follow-up appointment process in place. Patient History and Integration of Data: Integrated records facilitate individualized care, which informs patients that the clinician remembers and cares about their health history. It can prove to be an immense driver for repeat bookings. How does Clinic Management Software help Increase Repeat Bookings? Let’s see in depth how this software can improve patient return directly. Automates Follow-Up and Recall One of the biggest strengths of automated patient recall systems is that they eliminate human error and provide timely contact. Whether chronic illness reviews, vaccinations, or follow-up post-treatment, automating the process means no one falls through the cracks. For instance, dental offices frequently employ this to remind patients of cleanings every six months. Automating the recall process means clinics don’t have to manually track patients to bring them back regularly. Enhances Loyalty and Experience To increase patient loyalty in private practice, personalization is key. Health education content, frequent updates, and chat features help build confidence and bonds. They are part of a wider Patient engagement solutions strategy that enhances communication, stimulates feedback, and establishes long-term relationships. An active patient is more likely to feel looked after and thus more likely to book their next appointment. Reduces No-Shows No-shows interrupt timetables and waste time. Clinic management software dramatically minimizes this problem by using intelligent reminders. One study demonstrated that reminders by SMS cut no-shows by more than 25%. With repeated bookings via automated SMS, practices can remind, reschedule, and follow up—all without staff interaction. This dependability improves working efficiency and patient satisfaction, both of which lead to repeat visits. Increases Loyalty and Experience To build patient loyalty in private practice, customization is the key. With full access to patient histories, communication logs, and preferences, practitioners can provide personalized care. This makes patients satisfied and more likely to book an appointment in the future. Moreover, software solutions make it easy to conduct post-visit surveys. These assist in finding areas for improvement and make patients feel that their voices are heard, enhancing loyalty. Enables Strategic Marketing Effective digital marketing for private clinics can be integrated with the software, using email campaigns or SMS to notify patients about health tips, new services, or appointment openings. When patients regularly hear from their clinic in useful and non-intrusive ways, they stay connected and are more likely to return. Supports Growth Strategies A strong booking and follow-up system facilitates medical practice growth strategies through retaining existing patients, while also allowing for the ability to service new ones efficiently. Clinic software can provide reporting on booking patterns, patient testimonials, and campaign performance, allowing clinics to make informed decisions to grow and expand. How Clinic Management Software Facilitates? The following is a combined list of how Clinic management software benefits repeat bookings: Streamlines scheduling and rebooking Reduces no-shows with automated reminders Increases engagement with personalized communication Automates follow-up recalls Facilitates feedback gathering and service enhancements Increasing patient return rate with clear and consistent communication Syncs with AI healthcare innovations for predictive scheduling Facilitates real-time drug safety monitoring for patients on complicated medications Streamlines healthcare data integration with AI for enhanced patient tracking Supports telemedicine and
AI-Driven Pharmacovigilance: Revolutionizing Drug Safety Monitoring Pharmacovigilance is the study of the monitoring and evaluation of all adverse effects related to pharmaceutical products, and all of this has undergone a drastic transformation owing to the impact of Artificial Intelligence (AI) on this field. Traditional systems are important, but rather reactive and limited in scope. The rise of AI innovations in healthcare is changing the way the world manages drug safety with real-time, data-driven insights. Even countries like Pakistan tend to see Pharmacovigilance System Implementation that need to be implemented for a stronger AI in the Public Health infrastructure and improved patient safety. Understanding Pharmacovigilance By identifying, monitoring, and preventing ADRs, pharmacovigilance can maintain safety to the patient and public trust in medicines, especially upon the introduction of new drugs. A process through which adverse drug reaction notification can greatly increase public safety and trust in medicines. Pharmacovigilance in Pakistan is still developing in countries like Pakistan. It is evident in the growing interest by many health institutions in building better drug safety systems that conform to international standards. Traditional methods, however, seem to fall short on several challenges relating to speed, accuracy, and scope. Limitations of Traditional Pharmacovigilance Methods Conventional pharmacovigilance primarily relies on manual reporting, case analysis, and passive databases for recording adverse reactions to drugs. These enable underreporting, delays, and inconsistencies in the detection of adverse reactions to drugs. Certain incidents may not be reported by healthcare providers, whether owing to time constraints or due to sheer lack of awareness, thereby compromising the efficacy of the entire monitoring system. To add to that, these systems cannot withstand any further scaling with the current volume of healthcare data that continue to be generated from hospitals, pharmacies, and digital health platforms such as telemedicine and drug safety consultations. This becomes a bottleneck for real-time detection of emerging safety signals or effortless management of complex datasets. How AI is Transforming Pharmacovigilance? Artificial intelligence is throwing its weight on drug safety to mitigate various limitations in the above situations by automating the data collection, processing, and analysis processes. Machine learning in pharmacovigilance enables the identification of patterns from large datasets that facilitate the early detection of ADRs that may evade traditional reviews. Natural language processing (NLP) extracts relevant safety information from unstructured data sources, such as clinical notes, social media posts, and electronic health records. AI can merge different information sources to enhance real-time drug safety monitoring and predictive model building. Such AI systems in healthcare are capable of analyzing the patient’s genetic profile, lifestyle, and medical history for predicting Drug Reactions that would otherwise occur. This approach shifts pharmacovigilance from a reactive system to a proactive one regarding its intervention for improving patient outcomes. Book Free Demo Benefits of AI-Driven Pharmacovigilance ● Detection of ADRs at an Early Stage Millions of health records and reports on incidents may be rapidly analyzed by AI for untoward drug reactions. This will enable safety regulators or pharmaceutical companies to react promptly by sending safety announcements or amending drug dosage, etc. ● Enhanced Scalability and Efficiency Automation shortens the time we need to analyze extensive sets of data on pharmacovigilance, thus alleviating the pressure on human resources. This is particularly a huge blessing in nations like Pakistan, where there is hardly any resource for carrying out manual assessment. ● Enhanced Decision-Making With a modular form of AI, decision-making is aided by real-time dashboards and actionable insights to healthcare professionals and regulators. This enhances decision-making to combat safety threats at an early stage of their development. ● Increased Patient Safety By using artificial intelligence, hospitals can enhance Patient Safety through AI with pharmacy data and telemedicine platforms. Artificial intelligence highlights high-risk drugs or interactions, thereby decreasing patient harm. ● Support for Health Initiatives Public AI plays an important role in identifying trends in the public health sector, whether drug misuse or areas of regional side effects, which, when monitored and predicted better, can be useful in designing more effective health policy interventions. ● Convergence with Wearable and Mobile Health Data AI systems typically aggregate and analyze data received from wearable devices and integrated health applications for tracking Adverse Drug Reaction Detection incidents outside clinical settings. Thus, the entire health picture becomes better visible for a patient. It allows real-time, continuous monitoring of drug safety. ● Predictive Assessment of Patients on an Individual Level By better individualizing risk profiles, including genetic evaluation, age, gender, comorbidities, and drug history, artificial intelligence through machine learning in the field of pharmacovigilance can provide risk assessments at the individual level. Hence, personal drug safety improvements in intervention, along with better treatment efficacy and reduced side effects. ● Compliance Support from Regulatory Agencies AI technologies make the financial house easier to recognize to fulfill local and international regulatory requirements through a much more reliable reporting and documentation system created for the pharmaceutical industry and healthcare providers. Automation reduces human error and provides reliability, making pharmacovigilance reporting consistent. ● Strong Clinical Trial Monitoring Automatic processing of participant data leads to a quicker detection of ADRs using AI in the course of clinical trials. This advances safety when conducting trials and facilitates quicker approvals of promising treatments. ● Improve Communication Healthcare Provider AIs can provide notifications and alerts for doctors and pharmacists at the time real-time events when there is an incident likely to warrant a follow-up. Thereby improving communication, the readiness for quick clinical decisions will significantly minimize the possibility of complications. Challenges and Ethical Considerations These AI healthcare innovations are promising in nature, but they have their challenges and some points of ethical concern. ● Data Privacy and Security About the need for AI to enhance pharmacovigilance, a huge volume of sensitive health data is paramount. Privacy and security become a major issue in bringing Healthcare Data Integration with AI under the wings of AI because mishandling of the data can dent public trust. ● Bias in Algorithms “The
What You Must Know About Patient Engagement Solutions? In the rapidly evolving healthcare landscape of today, Patient Engagement Solutions are arising to transform how and when care is received and embraced. These solutions are customised to facilitate meaningful interactions between patients and healthcare professionals through technology as a way of informing, empowering, and actively engaging people with their health. From AI platforms to health communication platforms tailored for every patient, medical advancements are fast redefining the medicine of the future today. From improved communication to enabling chronic disease care to maximizing learning, patient engagement is at the core of Improving Patient Satisfaction with Technology. With an oppressive system, digital platforms are streamlining processes, closing gaps in care, and building trust. The Importance of Patient Engagement in Modern Healthcare In value-based care, the measures are outcomes, and patient engagement is number one. With Patient Engagement Solutions, healthcare is a two-way process where patients are not passive patients but informed decision-makers. These solutions ensure that healthcare is accessible and engaging by providing services such as real-time messaging, personalised dashboards, mobile reminders, and patient portals. They ensure that preventive care is achievable through timely reminders for check-ups, screenings, and vaccinations. Aside from that, Patient Communication Tools in Healthcare are setting the pace when it comes to shattering barriers of communication among patients and caregivers, most surprisingly in home-care or outpatient contexts. From telemedicine consultations to secure messaging software, the tools guarantee that the patient is never left in the dark regarding his or her health status. Effective Patient Engagement Strategies To truly engage patients, clinicians need to embrace reflective, thoughtful practices that transcend boilerplate outreach. Targeted Patient Engagement Strategies include constructing rich, contextually grounded interactions based on patient behavior, preference, and demographics. Effective strategies are widely used by healthcare organizations as described below: Segment patients by risk level, age, and communication style Leverage patient feedback to enhance service delivery Construct mobile-first systems for communications Offer culturally sensitive educational materials Use automated workflows for follow-up and post-discharge care A strategic plan not only boosts enhanced patient Satisfaction with Technology but also minimizes readmissions and maximizes compliance rates. Patient Engagement Drivers 1. Communication & Educational Tools Patient education is the key to patient empowerment. Web-based tools like apps, video, symptom checkers, and individualized care pathways break information into smaller pieces. They also empower patients more and stress them less. Patient Education and Engagement Tools facilitate learning outside of the care environment, from taking medication to post-operative follow-up. These solutions are designed to provide patients with a firm understanding of their condition, treatment possibilities, and what it will take to get well. Digital Health Engagement Platforms, in turn, offer seamless access to records, reminders, live chat help, and health advice, which are simple to share and invite patients to self-manage. 2. Patient Portals and Mobile Integration Personal health information access is among the leading causes of participation. Patient Portal Integration provides patients with secure access to test results, medical history, prescriptions, and appointment dates. When used with mobile applications, it provides a single, uncomplicated experience. Furthermore, Mobile Apps for Patient Engagement provide an immediate means of using healthcare systems anywhere, anytime. Push notification for medication refilling is easier, and ease dominates, a contributing factor toward the perpetuation of hectic lives. Main Features of the Patient Engagement Software Today’s engagement platforms are packed with features and very customizable. Key Patient Engagement Software Features include: Real-time Patient Communication for Healthcare through video consults, live chat, and secure messaging Remote Patient Engagement Solutions for long-term care, telemonitoring, and home-based diagnosis Seamless integration with Healthcare CRM and Patient Retention software for active patient follow-up Personalized alerts and Custom Healthcare Communication by treatment plans Voice and chatbot support for repetitive question handling Ease of use through mobile and web-based access All these features make it easier for a more streamlined, personalized delivery of care. Enhancing Patient Experience with Technology The digital experience is as relevant as individual one-to-one treatment. Healthcare services need to be easy, agile, and accessible. Enhancing Patient Experience through Technology means reducing friction and delay and making information more accessible. For example, wearable devices that track vitals and present them to healthcare providers help detect issues early. Virtual visits are made convenient without compromising care quality. Digital consent forms, billing, and automated feedback save administrative time while keeping patients informed and engaged. By integrating Patient Engagement Solutions into these touchpoints, providers build a better, more human-centered healthcare experience. Role of AI and CRM in Modern Patient Engagement AI is increasingly contributing to healthcare engagement. The Role of AI in Patient Engagement includes natural language processing for chatbots, predictive analytics for determining patients at high risk, and content personalization for engagement campaigns. The Role of AI in Healthcare is evident in how it analyzes patient behavior patterns to send timely, context-sensitive messages or reminders. For instance, if a diabetic patient hasn’t logged a blood glucose level in a few days, the system can issue a gentle prompt or initiate a call to connect them with a nurse. Furthermore, Patient Retention and Healthcare CRM offerings maintain patient information for optimal retention and interaction. They can tailor contact by patient characteristics, history of visits, and even level of satisfaction, guaranteeing continuous, customized communication. Personalized and Real-time Communication One of the most potent Patient Engagement Solution differentiators is the ability to communicate effectively and in real-time. Some of the most critical elements of personalized, Real-time Communication in Healthcare are listed below: AI-driven care reminders, personalized by health status Multilingual SMS/email messaging for multilingual populations Virtual assistant robots for appointment booking and FAQ Personalized video messages or voice messages from doctors after treatment Feedback-informed outreach for continuous quality improvement Wearable device
Telemedicine as a concept has in the recent past been on the spotlight as an effective modality of delivering healthcare especially in the management of chronic diseases such as telemedicine for heart disease. This paper therefore seeks to give a comprehensive overview of telemedicine for heart disease and may be very useful for patients or caregivers who wish to understand the trends or advancements in the field of telemedicine. The Rise of Telemedicine Telemedicine sometimes also referred to as telehealth, is a modem form of practicing medicine where contact with patient is made through telecommunication technology. Telemedicine has advanced over the years with technological evolution, and has thus improved in its quality and availability, changing the healthcare industry. Patients are in a position to directly interact with healthcare professionals and get experts advise or any medical opinion they require without being restricted by geographical barriers which improves on convenience and flexibility. The vale of telemedicine can be paramount for the patient with heart diseases. Firstly, it offers an ultimate convenience given the fact that its services do not require a visit face-to-face. It can reach out to large numbers of patients and dispense consultation to them without having to travel to their homes, which can be time-consuming and at times, tiring for both the patients and the healthcare provider. This convenience also promotes a desirable level of patient interaction and repeated visits that are key to compiling with continuous care illnesses. Book Free Demo Key Services Telemedicine for Heart Disease Management 1-Virtual Consultations Patients can directly discuss with cardiologist and other healthcare practitioners using the latest video calling solutions. Such virtual visits provide thorough reviews concerning the client’s disease state, the symptoms, prescriptions, and associated recommendations concerning the client’s daily practices. By the end of the visit, patients can ventilate on the issues that bother them and get individualized management plans being given. 2-Remote Monitoring Devices Smartwatches and mobile health apps are named as the wearable technologies that have significant roles in remote heart disease management. These devices monitor distinct markers such as pulse rate, blood pressure, and the level of activity allowing physicians to analyze the cardiovascular health of the patient. This data is also useful for the healthcare providers to access this data from a distance enabling them to monitor the patient’s status and be in a position to offer timely help whenever a complication or even worsening of the symptoms of this disease is spotted. 3-Telepharmacy Services Medication management is another crucial area in the treatment of heart diseases, whereby telemedicine provides a telepharmacy service to help patients. It is essential for a patient to request a refill on his or her prescription medicines, get advice on any medicines that may be taken together or information concerning any problems or side effects a patient may be experiencing from any medicine. Transitioning to Telemedicine: What Patients Need to Know 1-Technology Requirements Patients have to have equipment like a smartphone or a computer tablet connected to the internet in order to have telemedicine appointment. The patient should ensure that they check the technical specifications of the telemedicine application to determine whether they have all the software, hardware, and other features they need before agreeing to download the application and schedule the appointments. 2-Privacy and Security This is particularly important in telemedicine because patients and providers are essentially transmitting private medical info via electronic communication means. To ensure compliance with the privacy of their information, patients need to ask their care providers how they protect their information from unauthorized use. This entails ciphering measures, secure communication procedures and other aspects conforming to company and country protective. Ways of preserving the privacy and the sanctity of patient information is crucial in propelling the trust of patients and meeting the legal requirements of care organizations. 3-Insurance Coverage Telemedicine is gradually becoming part of the insurance plan for the management of heart diseases, whilst insurance coverage for telehealth services remains in a fluid status dependent on the insurance service provider and options of the various telehealth services to be availed. It’s the patient’s responsibility to contact their insurance provider and understand whether such treatment is available, free of charge or they will need to pay in form of co-payment or out of pocket payment. It’s important to note that some insurers may need pre-authorization for telemedicine teleconsultation or restrict coverage to specific physicians or services. Effective communication with the insurer also plays into not having to deal with surprise expenses added onto a patient’s bills and navigating insurance can only be reinforced by patients making an attempt at understanding the details of their policy beforehand. Conclusion It is therefore cost effective, patient centered and become a perfect model of telecommunication for managing heart diseases. Through integrating information technologies and using telecommunication modern means telemedicine provides access to narrowly-profiled treatment, enables consistent monitoring, and creates the necessary basis for effective prevention of heart diseases. Based on the progression of telemedicine and its endorsement as an appropriate method of delivering care, the use and impact of this technology for heart disease patients has the potential of bringing about favorable change and lead to the improvement of quality of life of numerous patients. Adoption and implementation of telemedicine serves as part of a multilayered management of heart disease hence increasing the chances of healthier outcomes, lighter pockets and happier patients. FAQs 1-What is telemedicine, and how does it work for heart disease? Telemedicine, or telehealth, is a modem method of diagnosing and treating patients without a physical contact with them utilizing telecommunications technology. In heart disease management, teleconsulting can be used where patients can easily interact with cardiologists as well as other doctors through online platforms. Patients can share experiences on products and services, seek medical advice, and get their health checks done, including monitoring vital signs through wearable technology and MH applications. Through the expansion of telemedicine technology, the chances of people with heart diseases getting adequate care are high, and they are closely
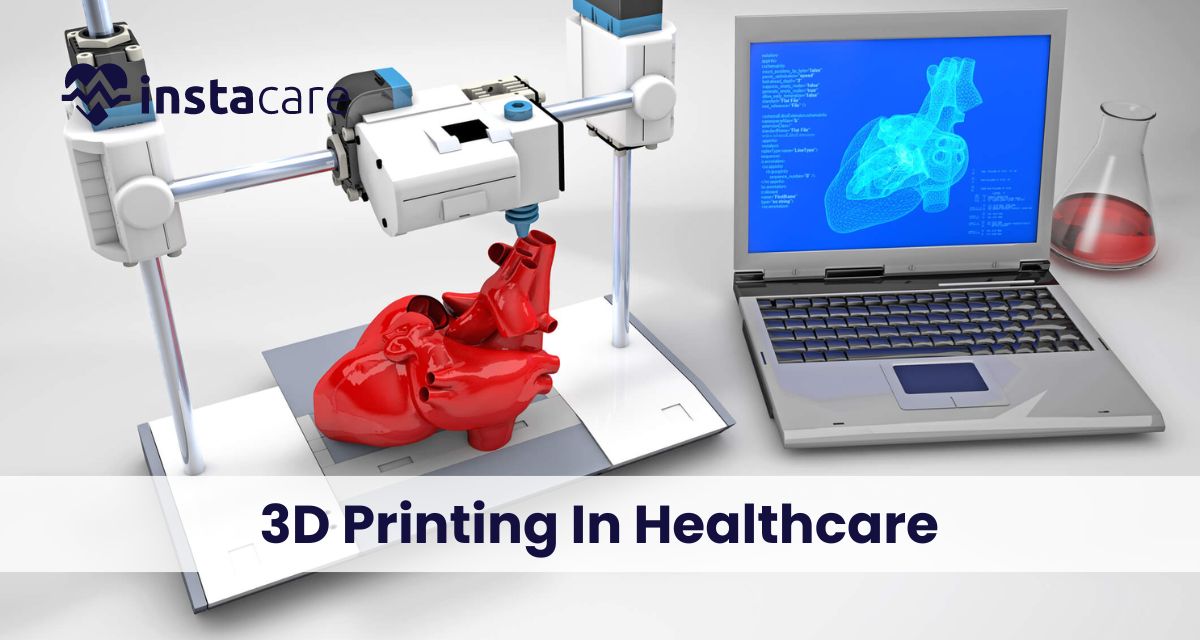
All You Must Know About 3D Printing In Healthcare Making It Personal First known term of 3D printing in Healthcare, or as it is authoritatively named, added substance producing, can be followed back to the 1980s. Since its development it has been placed in different applications in ventures, for example, the clinical and medical services industry where it has heaps of potential. It has even been applied in the growth of replacement organs, prosthetics and other medical equipment and applications. In this article I will explain more about the possibilities of using additive manufacturing in the sphere of medicine. Regarding this technology, let us consider the benefits, limitations and issues involving its deployment in this sector of the medical field; we shall also briefly look at FDA guidelines on the safety of products made from additive manufacturing for use in the medical sector. Finally, we will look into other uses of Additive manufacturing in the present and future. What Is 3D Printing In Health Care? Manufacturing is the process of transforming materials into an object and 3D printing is a unique way accomplishing this process in a manner that opposes the conventional approach. Unlike the traditional manufacturing techniques which require a block of raw material to be cut, sculpted, or milled to create the desired final product, 3D printing constructs objects from a digital blueprint by adding successive layers of a chosen material such as plastics, metals, or ceramics. These objects are created from digital files such as Magnetic Resonance Imaging (MRI) or computer aided designs (CAD), and are versatile when it comes to changes during the production or planning. There are hundred types of 3D printers in the market that are both inkjet and laser and come in models suitable for home or industrial use for the manufacturing of many types of goods. Custoized Prosthetics An Unrest in Appendage Substitution 3D printing has introduced another period in the development of prosthetics, offering a groundbreaking way to deal with making redid appendage substitutions customized to every individual’s particular life structures. This momentous progression has re-imagined the ordinary techniques for prosthetic assembling, delivering a scope of advantages that essentially lift the solace and usefulness of prosthetic gadgets. Customization And Accuracy One of the vital benefits of 3D imprinting in prosthetics is the unmatched degree of customization it offers. By using progressed checking and imaging advancements, prosthetists can catch exact estimations and shapes of the remaining appendage, empowering the creation of prosthetic parts that impeccably line up with the singular’s remarkable life systems. This degree of customization guarantees a dominant fit and solace, tending to the impediments of off-the-rack prosthetics. Improved Solace And Usefulness Fit, comfort, and functionality are frequently issues with traditional prosthetics. With 3D printing, the prosthetic attachment and parts can be custom-made to the singular’s particular requirements, bringing about a more agreeable and useful prosthetic arrangement. This customized approach limits issues like skin bothering, inconvenience, and unfortunate arrangement, offering clients a prosthetic gadget that consistently incorporates with their body and upgrades their versatility and personal satisfaction. Developed Style And Plan Adaptability 3D printing considers multifaceted and stylishly satisfying plans, offering people the chance to communicate their own style and inclinations through their prosthetic gadgets. The flexibility of 3D printing empowers the formation of prosthetic appendages that have the capability to ideally mirror the singular’s character and personality, advancing a feeling of strengthening and certainty. Book Free Demo Availability And Moderateness Many amputees have faced significant obstacles due to the high cost and lack of availability of individualized prosthetics. 3D printing can possibly address these difficulties by smoothing out the assembling system and decreasing creation costs, making redid prosthetics more open to a more extensive populace. Propelling Recovery And Prosperity Individuals who have lost limbs may benefit from the personalized nature of 3D-printed prosthetics’ rehabilitation and well-being. By giving prosthetic arrangements that are custom fitted to their interesting necessities and inclinations, 3D printing adds to improving the by and large physical and close-to-home prosperity of prosthetic clients. Personalized prosthetics have undergone a paradigm shift as a result of 3D printing, which has revolutionized the manufacturing process. This headway tends to the restrictions of conventional prosthetics and engages people with appendage misfortune by furnishing them with altered, agreeable, and utilitarian arrangements that line up with their particular physical prerequisites. Careful Preparation And Practice With 3d Printing in Healthcare Models Fastidious Methodology Readiness: Specialists are outfitting the force of 3D printed models to design and plan for complicated and high-stakes methods carefully. Surgeons can effectively visualize and evaluate the surgical site, anticipate potential obstacles, and plan the precise execution of the procedure by utilizing these patient-specific 3D models. Improved Accuracy And Ability Refinement The usage of 3D printed models permits specialists to refine their procedural strategies and gain important active involvement with a recreated climate. As a result, surgical errors are reduced and patient outcomes are improved thanks to this practice’s significant improvement in precision and proficiency. Lessening Careful Dangers The pre-careful utilization of 3D printed models supports distinguishing and tending to expected difficulties or varieties in understanding life structures, in this manner, moderating dangers related to the method. This proactive methodology limits the probability of blunders during a medical procedure and advances more secure, more successful mediations. Worked On Persistent Results Through fastidious preparation and rehearsed planning with 3D printed models, specialists can accomplish increased degrees of readiness, prompting work on persistent results, diminished inconveniences, and improved by and large careful achievement rates. Progressing Careful Schooling Furthermore, 3D printed models act as significant instructive devices, giving a stage to careful students to master and refine their abilities in a reasonable and material way, at last adding to the headway of careful schooling and capability. In outline, the joining of 3D printed models in careful preparation and practice enables specialists to fastidiously plan, refine their abilities, and at last lift the norm of patient consideration through upgraded accuracy, decreased blunders, and worked on careful results. Customized Prescriptions With 3D printing, the
Pushing The Boundaries Of Healthcare Technology – Tips & Strategies Development has turned into an imperative instrument in medical services in the quickly advancing current scene. The blend of state of the art advancement with cutting edge care might have the option to push the limits of what is conceivable in clinical benefits, from working on understanding thought to adjusting legitimate cycles. In any case, tackling these likely calls for cautious preparation, imaginative reasoning, and a promise to beat snags. This post will look at some fundamental techniques and devices for capitalizing on medical services development. 1-Harnessing The Potential Of AI And Ml In Healthcare Technology By utilizing information investigation to spike bits of knowledge and innovativeness, man-made brainpower (computer based intelligence) and AI (ML) advancements can possibly totally change the medical services industry. Examining Extensive Data Sets Huge information in medical services, like hereditary data, demonstrative imaging, and patient records, is best handled by man-made intelligence and ML. Man-made reasoning (computer based intelligence) frameworks can track down examples, connections, and patterns in this information that probably won’t be noticeable to human eyewitnesses. Forecasting Abilities Prescient examination is one of the most astonishing purposes of computer based intelligence and ML in the clinical field. These advancements can distinguish individuals that are in danger, gauge patient results, and even anticipate sickness flare-ups by concentrating on authentic information. Medical services experts can make an early move thanks to this prescient expertise, which might assist with deflecting ominous events and upgrade patient results. Tailored Care Programs By tweaking treatment regimens for every patient, artificial intelligence and ML can work with altered medication. Computer based intelligence calculations can distinguish the best game-plan for every patient by analyzing hereditary, ecological, and way of life factors. This amplifies therapeutic viability and limits unfriendly impacts. Improving Judgment Making By integrating simulated intelligence and ML into clinical methodology, clinical faculty might get ongoing choice help. Computerized reasoning (man-made intelligence) calculations can enhance the information on human experts by giving proof based thoughts for finding, treatment determination, and care for the board. Making Resource Allocation More Efficient Medical care frameworks may likewise enhance asset assignment with the utilization of computer based intelligence and ML. Through the examination of patient stream, asset use, and functional failures, these advances can pinpoint regions that require improvement and upgrade processes, which thus prompt expanded efficiency and diminished costs. Increasing Patient Results Eventually, quite possibly integrating man-made intelligence and ML into clinical practice might upgrade patient results all around the medical care range. Medical services professionals may now offer greater consideration and further develop patient joy as a result of these innovations, which empower more exact determination, individualized therapies, and informed direction. Book Free Demo 2-The Importance Of Data Security And Privacy Protecting patient information is turning out to be progressively significant for medical organizations when medical services information is steadily moving into computerized designs. Strong Security Measures Implemented To improve information security, medical care associations need to utilize sweeping safety efforts that incorporate interruption location frameworks, access limitations, and encryption. By lessening the chance of information breaks and forestalling unapproved access, these safeguards help safeguard patient data’s classification and uprightness. Complying With Tight Privacy Laws Medical organizations need to ensure they are in accordance with severe protection regulations like the Health care coverage Convey ability and Responsibility Act (HIPAA). Patients’ and medical care suppliers’ trust is expanded when these norms are followed since they ensure that patient information is taken care of with the most noteworthy mystery and straightforwardness. Protection Of Private Data Solid information administration frameworks are important for medical care organizations to safeguard delicate information during its entire life expectancy. This involves setting up methodology for social occasions, putting away, sending, and disposing of information as well as performing routine reviews and appraisals to find and fix weaknesses from the get-go. Building Trust Medical care associations show their commitment to keeping up with moral principles and defending patient secrecy by putting a high need on information security and protection. This reinforces the patient-supplier association by empowering trust among patients and medical services experts as well as giving patient’s confidence in the genuineness of the medical services framework. 3-Cultivating Innovation with Healthcare Technology In Organizations Innovations ought to take on the substance of the medical care association that looks to change to the ongoing climate of medical services innovation and conveyance frameworks. Engaging Employees And Encouraging Them To Think Creatively It is basic that representatives are permitted to break free and all the more significantly think about new developments in their profession. HCOs ought to lay out an essential way to deal with ideation through planning open gatherings, hack-a-thons, and development rivalries where the laborer can submit and plan new answers for recent concerns. Experimenting With Emerging Technologies Another need is an emphasis on the utilization of late improvements in innovations for propelling medical services conveyance. Corporate elements ought to support the testing and utilization of advancements like man-made consciousness, telemedicine, and wearable gadgets to improve the conveyance of workforce clinical consideration, increment effectiveness, and overhaul inward cycles. Challenging The Status Quo As indicated by the data given, there is a need to continuously have a specific degree of interruption to the typical working of the medical services industry. It ought to turn into a standard practice in associations where representatives prompt a change and begin inquiring as to why things are finished in a specific way. Along these lines, and through introducing novel thoughts that pay attention to the impression of existing practices, medical services associations can foster new systems for advancement. Fostering Creativity And Collaboration Advancing techniques that animate thought age and participation is particularly significant in the medical care concern. Pioneers in associations ought to shape groups with laborers whose foundations and aptitude are very not quite the same as each other in order to streamline collaboration. Through powerful correspondence with others in the medical services associations, quite possibly the best component that can be rehearsed is individuals’