AI in SaaS: Artificial Intelligence and Its Impacts on the Software Industry The marriage of artificial intelligence and Software as a Service (SaaS) is transforming how digital platforms run, expand, and build value. The dizzying technology landscape today does not just mean that AI is the evolution of back-burner SaaS-it is a revolution. From automated tasks to forecasting customer wants and delivering tailored experiences, AI use cases in saas solutions are changing the way businesses engage with software. From customer support to marketing, analytics, or product innovation, the SaaS application of artificial intelligence is tremendous and revolutionary. Here in this blog post, we are going to talk about the major benefits, real-world applications, and the future of AI for SaaS. What Is the Role of AI in SaaS? Effectively, AI in SaaS is intelligent software. A matter of connecting machine learning, natural language processing, and predictive analytics in saas into cloud application software. Why? To automate, learn, and personalize user interactions. Role of AI in saas industry is being increasingly integrated into SaaS apps to: Learn from user behavior and trends Automate routine tasks such as onboarding or support Offer real-time decision-making abilities Offer predictive business strategy insights AI adoption in SaaS businesses has come an incredibly long way from being an experimental feature to being one among the primary pillars of scalability and innovation. Benefits of AI in SaaS Benefits of AI in SaaS are all phenomenal, not just cost and automation, but even customer satisfaction, product fine-tuning, and strategic decision-making. 1. Smart Customer Support One of the most prominent applications of AI is customer care. AI-driven customer support in saas applications employs intelligent chatbots to assist customers in real time, address issues, and route difficult problems to human agents. This reduces response time and provides support 24/7. 2. Augmented Decision-Making With SaaS predictive analytics, businesses are able to predict churn, identify upsell opportunities, and track customer satisfaction levels precisely. AI technology sifts through mountains of data in seconds to identify patterns and behavior that might otherwise go unnoticed. 3. Operational Efficiency AI automation in saas allows business enterprises to automate back-end activities such as data entry, invoices, and reports. Automations provide teams the chance to shift focus towards strategic work instead of drudge work. 4. Tailored User Experience AI allows SaaS solutions to tailor dashboards, recommendations, and content rendering based on individual user activity. It enhances engagement, retention, and happiness. 5. Scaling Without Incremental Burden With AI, SaaS products scale without the expense of operation doubling. From onboarding large numbers of new clients using AI operations to monitoring performance in real-time, scalability is done beautifully and effortlessly. Machine Learning in SaaS: Real-Time Learning & Adaptation Machine learning (ML) is one of the four pillars of artificial intelligence in SaaS. Machine learning in saas allows apps to learn from the way individuals interact with them, get better with time, and change dynamically as needs evolve. Examples: A sales platform can use ML to offer recommendations for best prices based on historical purchase behavior. A project management tool can forecast deadlines or risk based on historical trends. A content recommendation platform can be enhanced to recommend more in line with user interaction with articles or media. SaaS machine learning does not automate but enhance-smartly, optimizing platforms and maintaining competition intact in a live environment. AI in SaaS Marketing Riding the personalization wave, AI in SaaS marketing is a success story. AI enables the marketing team to: Segregate audiences based on behavior and engagement Automate lead nurture campaigns Measuring campaign performance in real-time AI-powered prediction of the most likely to pursue leads AI-powered marketing applications like chatbots, content engines, and A/B testing have become the secret sauce of the growth-stage SaaS company. AI-powered customer journeys provide more contextually relevant interactions and improved conversion. AI Chatbots for SaaS: Transforming Customer Engagement Chatbots are the most visible and most widespread application of AI tools for saas companies. From a CRM tool to helpdesk software to an HR tool, AI chatbots for saas are transforming communication. The chatbots: Process run-of-the-mill questions automatically Enable onboarding and simplify product use Collect past feedback and escalate when needed What distinguishes SaaS AI chatbots from the conventional bots is that they are learnable through conversation, context-sensitive, and get smarter every day. They offer smooth, almost-natural conversation experience without any human delay or limitation. Book Your Free Marketing Consultation AI in SaaS Product Development AI has revolutionized product development. AI is involved in the entire life cycle of a product from ideation and testing to updates and support in the SaaS era these days. The development in this field is astounding: Autotesting: AI technologies are able to find bugs and usability problems to speed up quality assurance. Feature prioritization: AI takes into account user activity and feedback to identify what’s the top-priority feature. Code generation and optimization: AI power at scale makes developers code, test, and optimize code better. AI and SaaS product development go hand in hand when it comes to releasing enhanced, faster, and more reliable updates driven by data and centered on users. How AI Is Transforming SaaS Models Apart from functionality and features, AI is also transforming the business and growth model of SaaS businesses. Some of the prominent how AI is transforming saas are: Usage-based billing: AI tracks usage patterns to design equitable and scalable pricing. Customer success predictions: Platforms can now anticipate probable-to-churn customers in advance. Smart integrations: AI APIs are now a part of SaaS platforms, and third-party solutions can blend
Micro SaaS: Business Model, Ideas, Examples & How to Get Started The Micro SaaS model has opened up opportunities for solo founders, developers, and small teams to start sustainable, profitable businesses without raising tens of millions of dollars in capital. Micro SaaS is unlike traditional SaaS, which tends to aim at big markets and needs large teams. Micro SaaS is lean, concentrated, and niche-based. Micro SaaS depends on automation and low infrastructure to produce value at scale. In this step-by-step guidebook, we will define Micro SaaS, special benefits of micro saas, money-making concepts, real-world applications, and how to start a micro saas business-even on a lean budget. What Is a Micro SaaS Business? Micro SaaS refers to tiny SaaS products built and operated by a single person or a group of several people. Micro saas product development tends to address a very niche user base, finding extremely unique problems with custom solutions. Consider Micro SaaS the lean SaaS, simplified, yet more agile, and often more bootstrapped. In contrast to enterprise SaaS businesses such as Salesforce or HubSpot, micro saas examples businesses don’t need to have massive sales teams or venture capital backing. They love recurring micro saas revenue model, low overhead, and high automation. They’re perfect for solo founders, digital nomads, or independent devs who love secure passive income. Key Features of a Micro SaaS Model Here are the common features of a Micro SaaS business model: Niche-specific: Solves a particular audience or pain point that is largely neglected by big SaaS players. Bootstrapped: Founder(s)-controlled and non-venture capital-backed. Low overheads: Low resource intensities, often single-handed operations or small virtual team. Recurring revenue: Often associated with monthly or annual subscription-based pricing. Automated operations: Leverages automated customer onboarding, billing, support, and update tools. Simple tech stack: Often built over low-code environments or light frameworks. Owner-led: High autonomy and flexible operation. Developers, marketers, and founders prefer such traits when searching for freedom and scalable business models. Why Micro SaaS Is a Super Business Model? There are numerous reasons why Micro SaaS companies are so popular nowadays: 1. Low Startup Costs You can start micro saas startups for a few hundred dollars. Most founders use existing skills and web-based software to build MVPs (Minimum Viable Products). 2. High Margins With low expenses and subscription income, profit margins can be wildly profitable, usually 80% or higher. 3. No Scale Necessary You don’t need millions of customers. Hundreds of paying subscribers are enough to fund a lifestyle business. 4. Location Independent Because the work is automated, most Micro SaaS business owners work from anywhere. 5. Complete Ownership No investor needed, so you have maximum equity and control. 6. Perfect for Experimentation The model provides rapid product testing and pivoting. You can profitable micro saas ideas ideas faster with less risk. Successful Micro SaaS Ideas Here are some successful micro saas ideas to try: Newsletter Analytics Tool: For ConvertKit or Substack customers who need more advanced engagement metrics. Freelancer Proposal Generator: A software that freelancers would use to auto-generate personalized proposals. Online Course Progress Tracker: Plugin for online course creators to provide users with progress analytics. SEO Audit Widget: In-app website SEO audit solution for small business. Podcast Snippet Creator: Converts podcast audio into social media video snippets with subtitles. Client Feedback Manager: For agencies and designers to handle client feedback and approvals. Instagram Hashtag Organizer: Assists creators in organizing and cycling hashtags in a way that offers maximum reach. The majority of them are micro saas for developers, freelancers, or creators, individuals generally in the market for easy to use, affordable solutions. Book Your Free Marketing Consultation How to Create Your Own Micro SaaS Business? You do not need a technology degree and millions of dollars of capital to create your own Micro SaaS. Here is a straightforward roadmap: 1. Identify a Niche Utilize communities such as Reddit, Indie Hackers, or Twitter to learn about persistent pain points. Choose micro SaaS niche selection through underserved group discovery. 2. Validate the Problem Don’t create anything before speaking with potential users. Survey or directly interview to validate demand. 3. Build an MVP Launch on low code micro saas platforms like Bubble, Glide, or Webflow, or create a lightweight app using Node.js, React, or Firebase. 4. Setup Payment & Onboarding Add Paddle or Stripe for subscriptions. Auto-onboard with email series and help docs. 5. Launch & Promote Piggyback product onto nearby forums, blogs, and Product Hunt. Provide lifetime deals or early-bird discounts to get started. 6. Gather Feedback and Polish Polish based on user feedback. Release features incrementally, not app bloat. Bottlenecks of Bootstrapping Micro SaaS While it has its benefits, bootstrapping Micro SaaS does have some limitations: Support burden: Your customer support with no support team. Churn management: A rising churn rate from user cancellations hurts revenue and signals value concerns. Scaling limits: You can’t scale indefinitely without hiring employees. Marketing challenges: You’re forced to wear many hats, developer, marketer, and founder. Security & compliance: It’s your responsibility to make user data secure and GDPR-compliant. All these problems are solved in successful micro SaaS businesses by automation, outsourcing, or collaboration. Tools & Tech Stack Recommendations Following are crucial tools to construct and operate a Micro SaaS product: Frontend: React, Next.js, Vue.js Backend: Firebase, Node.js, Supabase Database: PostgreSQL, MongoDB Payments: Stripe, Paddle, Gumroad Authentication: Auth0, Clerk, Firebase Auth Customer Support: Crisp, HelpScout, Intercom Analytics:
SaaS Architecture: Design for Scalable Multi-Tenancy & Best Practices Increasingly, business is being taken to the cloud, and Software as a Service (SaaS) remains the ubiquitous software delivery platform. Since the foundation of any successful SaaS application is its architecture, the blue-print which specifies how the application behaves, scales, and acquires customers at affordable cost, product managers, CTOs, and SaaS businessmen/entrepreneurs must at least have a fundamental knowledge of SaaS architecture to develop good, scalable software. This tutorial addresses what is SaaS Architecture, its fundamental structure, design patterns, and best practices, typically under multi-tenant SaaS architecture and scalable architecture. What is SaaS Architecture? SaaS architecture refers to the application design of a computer program application accessed over the internet on a subscription basis. Unlike desktop on-premises application software, a SaaS application design offers easy access to the application from anywhere remotely, typically using a browser. The key characteristics of SaaS software architecture are: Cloud-hosted central hosting User access on a subscription basis Periodic maintenance by providers regularly Handling of fluctuating loads through scaling SaaS architecture, in a sense, prescribes how the system needs to behave in order to process users, data, scaling, and performance in the best possible way without losing out on isolation and security. Multi-Tenant SaaS Architecture: The Core Model One of the shared characteristics of most SaaS applications is a multi-tenant SaaS architecture, in which a single instance of the application serves numerous customers (tenants) and associated data and user-specific configuration. Why Multi-Tenant SaaS Architecture? Cost Effectiveness: Shared infrastructure = less expensive hosting. Ease of Maintenance: Single global patches and not by each deployment. Scalability: Less resource management as tenants increase. Single-tenant vs multi-tenant SaaS virtualized SaaS architecture is very different, however. Single-tenant SaaS is more expensive and more complicated virtualized separation and single customer assignment of assets. Both are selected by business and regulatory necessity and by end-user expectation. SaaS Architecture Components Effective SaaS backend architecture is built on several plain ingredients, which interoperate quite well: Application Layer: Business logic and user interface through which the customers were handled by the platform. API Layer: Inter-service communications, in the majority of instances through REST or GraphQL APIs. Data Layer (SaaS Data Architecture): Data storage, data retrieval, and data security. Data partitioning is used to segregate tenant data in a multi-tenant SaaS architecture. Authentication & Authorization: Used for deployment for multi-tenancy to control user access as well as fraud authentication on sensitive data. Monitoring & Analytics: Application performance monitor software, usage monitoring, and system health monitoring. These hardware building blocks of SaaS architecture are the basis for a secure, scalable, and successful application. Scalable SaaS Architecture: Design Principles Scaling makes a SaaS platform performance-optimized to be capable of supporting more users, data, and transactions without a reduction in performance. A scalable SaaS architecture is based on the following: Horizontal Scaling: Scaling servers or instances rather than hardware upgrades. Stateless Services: Support services to be replicated on many nodes regardless of server-side state. Load Balancing: Distribute traffic on, with no bottlenecks. Elastic Cloud Resources: Use cloud environments like AWS, Azure, or GCP for on-demand scaling. Cloud-native architecture makes cloud SaaS architecture able to offer dynamic scaling and resource management according to real-time actual demands. Book Your Free Marketing Consultation SaaS Architecture Patterns to Comply App developers must employ established and reliable SaaS architecture patterns while developing scalable and fault-tolerant systems. They are: Microservices in SaaS Architecture: Loose decoupling of the app simplifies development, scalability, and deployment. Service-Oriented Architecture (SOA): Services are reused to enable sharing of data within a network. Event-Driven Architecture: Services share data in the form of events to enable scalability and decoupling. Patterns support quick development, continuous integration and delivery, the most important to SaaS success. Microservices in SaaS Architecture Microservices in SaaS architecture revolutionized the implementation and deployment of SaaS platforms. Breaking down large applications into lean services, easy to deploy, and loosely coupled, businesses gain: Deployment Speed: New feature deployed through continuous deployment. Scalability: Each of the services is scalable in itself. Fault Isolation: The whole system does not fail if a service fails. Microservices add additional complexity in managing data, service discovery, and orchestration that has to be met by a solid design. SaaS Architecture Best Practices Long-term success, scalability, and customer satisfaction are achieved through the application of SaaS architecture best practices. Some of the best practices guidelines include: Design Multi-Tenancy from Day One: It is expensive and time-consuming to implement multi-tenancy afterward. Adopting DevOps & Automation: Real-time updation and reliability require constant deployment, monitoring, and integration. Put Security & Compliance First: Encrypt data in motion and at rest. Provide strong authentication controls and regular auditing. Optimize SaaS Data for High Performance: Use correct partitioning mechanisms, shared database with tenant ID, schema per tenant, or database per tenant, based on size and isolation needs. Make API-First Development the Default: APIs must be versioned, secure, and documented to allow third-party services and integrations. Track & Analyze Usage Patterns: Use monitoring tools to infer usage, customer behavior, and potential bottlenecks. Design for Failure: Put retries, fallbacks, and circuit breakers in place so fault-tolerant services are a reality. By these SaaS architecture best practices, organizations will prevent downtime, improve the user experience, and provide scalability. SaaS Platform Architecture: Cloud-Native Principles Cloud-native components and services are used extensively while developing SaaS platforms these days. Cloud SaaS architecture includes: Containerization (e.g., Docker): Simple deployment and scaling. Orchestration (e.g., Kubernetes): Execute containerized applications in clusters. Serverless Computing (e.g., AWS Lambda): Ideal for tiny, lightweight computations and decreasing operational costs. Managed Databases: Cloud vendors provide secure, scalable database as a service to SaaS applications. All these technologies enable SaaS providers to devote less time to less infrastructure management and more to application development. SaaS System Design: Performance vs. Cost The optimal SaaS system design is a performance-cost-complexity balance. Performance: Accelerate with caching, content delivery networks (CDNs), and query-opted queries. Cost management: Monitor
SaaS vs. PaaS vs. IaaS: Key Differences, Examples & Use Cases Explained Cloud computing transformed business operations for companies by offering computer resources with massive capabilities through the internet on demand. Instead of buying, owning, and maintaining physical infrastructure, companies now lease access to computer services, which is more agile and cheaper. Among the most popular cloud computing service models are SaaS (Software as a Service), PaaS (Platform as a Service), and IaaS (Infrastructure as a Service). Each supports business requirements differently with varying control, flexibility, and management. It is crucial that companies realize the difference between SaaS, PaaS, and IaaS before deciding to make an informed choice in choosing the most suitable solution for their IT infrastructure, whether for application development, warehousing data, or running business ventures. In this book, we will cover each model, the pros and cons of SaaS PaaS IaaS, key features of SaaS PaaS IaaS, show through live SaaS PaaS IaaS examples, and talk about best practices. What Is SaaS? Software as a Service (SaaS) is the most widely used and most used type of cloud delivery. SaaS delivers software applications over the web on a pay-per-use model. SaaS clients are not required to install, update, or maintain the software and consume SaaS products via a web browser or application. Examples of widely recognized SaaS include communication tools, customer relationship management (CRM), file sharing, and productivity. Google Workspace (Docs, Sheets, Gmail), Salesforce (CRM), Microsoft 365, Zoom, and Dropbox are some popular SaaS offerings. Common applications of SaaS include project collaboration, cloud services deployment models, customer service, HR management, communications platforms, and marketing automation. SaaS is suited whenever businesses need applications to be utilized instantly without the purchase of IT infrastructure or specific support. What Is PaaS? Platform as a Service (PaaS) offers a cloud platform to develop, test, deploy, and run applications without concerning the underlying infrastructure. Servers, storage, network, databases, and middleware are managed by the cloud provider in PaaS, and users design apps themselves. Some of the best-known PaaS instances include Google App Engine, Microsoft Azure App Services, Heroku, AWS Elastic Beanstalk, and IBM Cloud Foundry. They offer scalable application development environments that scale up as the application is being built. PaaS is commonly used to: Web and mobile app development API management and development Database administration Application hosting Continuous integration and delivery pipelines Those organizations that require innovation quickly without much concern for infrastructure use PaaS. It is a pre-set environment as an attempt to focus on writing code, testing, and deploying applications without wasting time. What Is IaaS? IaaS provides computerized infrastructure over the internet in virtual forms like servers, storage systems, networking connections, and virtualization layers. Unlike SaaS and PaaS, IaaS is able to provide total control to businesses so that they can structure and plan their IT infrastructure in whatever manner they desire. Leading IaaS providers are Amazon Web Services (AWS EC2 and S3), Microsoft Azure Virtual Machines, Google Compute Engine, DigitalOcean, and Oracle Cloud Infrastructure. These providers offer scalable infrastructure capabilities for hosting web sites, running enterprise applications, keeping data storage, and running high-computational requirement requests. IaaS is utilized in the following: Hosting high-level applications or websites Data storage and backup facilities Disaster recovery infrastructure Running big data analytics and artificial intelligence workloads Constructing virtual data centers for business corporation I completely agree with the fact that IaaS is the preferred choice of those organizations who possess on-premises IT organizations and prefer to own infrastructure, software stack, and security configuration. Book Your Free Marketing Consultation Key Most Differences: SaaS vs. PaaS vs. IaaS IaaS, PaaS, and SaaS are all cloud service deployment models, but they differ in terms of control, flexibility, and management responsibility. SaaS PaaS IaaS explained in this including the IaaS PaaS SaaS use cases. All this is managed by the cloud provider, application, data, runtime, storage, networking, and hardware. The customer just uses the software without any idea or even a concern about where or how it is being run. Enterprise use of SaaS, PaaS, and IaaS are different too for when to use SaaS vs PaaS vs IaaS. PaaS is in between SaaS and IaaS. Provider manages infrastructure, operating system, and runtime environment, and user manages application and data. PaaS is a platform for developing the application with emphasis on ease in application coding and deployment. IaaS provides the user with total control of the operating system, software, and data. The physical infrastructure, the servers, network, and storage, are taken care of by the provider. That leaves the company with total control of everything else from security policies to software updates. Choosing the Right Model: What Do You Need? Selecting the appropriate cloud model depends on your operations requirements, technical skills, and business demands. You may opt for SaaS if timely access to business applications is crucial without acquiring IT infrastructure. SaaS is particularly ideal for email, customer relationship management, document sharing, and communication tools. It is most suitable for businesses seeking cheap solutions with no maintenance and customization. PaaS is the way to go if app development and deployment is the business. If you have a development team that can command an environment to develop, test, and deploy apps without concern for servers or databases, then PaaS is an appropriate, scalable solution. Start-ups, software development businesses, and those piloting new digital products will see the most benefit from PaaS. Select IaaS in the event you wish to have absolute command over your IT infrastructure. Organizations with many, many more IT employees or dealing with sensitive data might use IaaS based on how flexible and adaptable it is. It is a good option for hosting business applications, virtual data center deployment, as well as building customized IT environments with bespoke configurations. There are
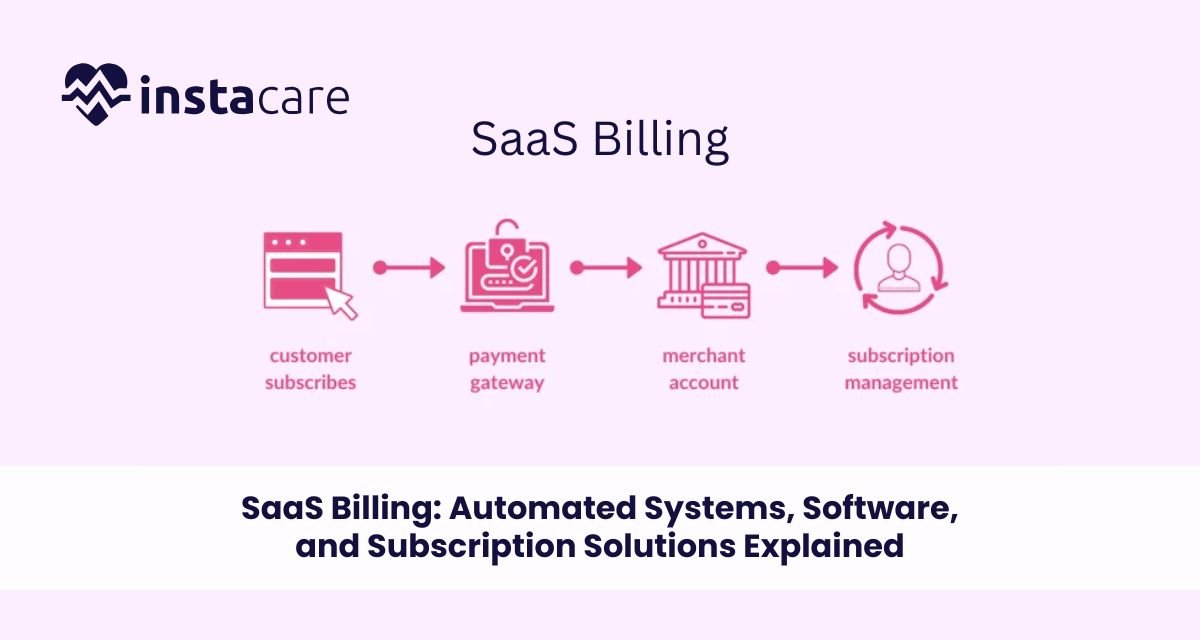
SaaS Billing: Software, Solutions, and Subscription Solutions Automated Defined Software as a Service (SaaS) business model has revolutionized how organizations provide value and interact with customers. Traditional software with one time payment does not come into play with SaaS business models in which organizations obtain recurring revenue from subscription plans, usage, or bundling fees. The revolution has brought with it the necessity for more effective automated SaaS billing platforms to enhance efficient operation, predictable SaaS revenue recognition, and customer satisfaction. Whether you’re a startup or an established SaaS company, understanding SaaS billing solutions and their role in your business is crucial to scale successfully and maintain financial health. What is SaaS Billing? SaaS billing refers to the procedures and processes through which customers are billed for software services monthly. SaaS subscription billing is distinct from standard billing procedures in that it supports flexible pricing, recurring charges, automated SaaS invoicing system, as well as subscription service-linked account management. SaaS billing procedures involve: Recurring SaaS subscription billing Automated remittance and invoicing Usage-based SaaS billing (metered billing) Tax calculation, discounts, and promotions Subscription management and upgrades In plain words, a SaaS billing platform allows convenient and effortless billing and payment for the business and customer. SaaS Billing Insights Recurring and Subscription-Based Models The recurring revenue model is the foundational concept of SaaS billing management. The customers pay monthly, quarterly, or annually for availing software services. Recurring billing for SaaS provides steady cash flow, predictable revenues, and improved customer retention. Metered and Usage-Based Charging Metered SaaS or usage billing SaaS pricing is applied primarily in SaaS companies when fees correlate directly with use of the service. Advanced tracking and autobilling infrastructure needs to be utilized to support it because billing must be done in real-time. Hybrid Billing Models Some SaaS businesses use both flat fee subscription and metered billing SaaS model. SaaS’s dynamic billing mechanism has to effectively address such variations to maintain billing accuracy and transparency to the customers. The Role Automated Billing Systems Play Automated SaaS billing is unavoidable for several reasons: Manual billing suffers from human error, delay, and compliance problems. SaaS auto-billing does away with them through auto-pay, time-saving for admins, and increased customer satisfaction. Core Billing Automation SaaS Solution Operations: Auto billing and auto payments: Does away with human error and improves cash flow. Subscription renewal and subscription management: Automates renewals, upgrades, downgrades, and cancellations. Usage tracking and metered billing: Allows for equitable billing of usage of services. Taxation and regulatory compliance: Complies with international tax laws, i.e., VAT and GST. Dunning management: Retry payments and notify customer for failed payments automated. Advantages of Automated SaaS Billing Systems: Improve accuracy and avert revenue loss Fosters customer trust through transparent billing Conserves time and operational expense Offers real-time analytics for customer and revenue activity Book Your Free Marketing Consultation SaaS Billing Software: Features and Benefits Main Features of SaaS Billing Software Flexible Pricing Configuration: Tiered pricing, freemium plans, and custom plans supported. Advanced SaaS Billings System: Invoicing automatically generated in real time with line item detail. Payment Gateway Integration: Multiple payment processors support for global acceptability. Subscription Life Cycle Management: Automatic trial period, renewals, cancellations, and refunds processing. Billings Analytics and Reporting: Revenue stream, churn rate, and customer lifetime value report in real time. SaaS Revenue Recognition Compliance: Automates revenue recognition in compliance with like ASC 606. Business Benefits of Using the Best SaaS Billings Software Scalability: Increasing bills with expanding customer base. Lower Churn: Effective billing and dunning save money and help reduce churn rate by retaining customers. Better Financial Projections: Reliable reports provide the ability to forecast revenues and cash flows. Customer Self-Service Functions: Allow customers to self-manage billing choices, change plans, or change payment units. SaaS Pricing Models 1. Flat-Rate Pricing A charge per period is levied by customers to access software features without restriction. Easy to charge but may be possible only for some customer segments. 2. Tiered Pricing Variable prices allow various levels of access or capability. Best suited to support more than one customer segment. 3. Usage-Based Billing (Metered Billing) Customers buy usage measures such as number of users, API calls, or used storage. Usage-based SaaS pricing models provide flexibility and fairness. 4. Freemium with Paid Upgrades Provide base functionality free and sell premium functionality through subscription. Must accommodate free and paying user bases within elastic SaaS billing infrastructure. 5. Hybrid Models Provide two or more pricing models to gain maximum flexibility and revenue optimization. Compliance and Security Considerations SaaS companies must comply with numerous payment, data privacy, and financial reporting requirements. Compliance Areas PCI-DSS Compliance: Secure handling of credit card transactions. GDPR and CCPA Compliance: Customer data privacy guaranteed. Tax Compliance: Tax calculation automatically calculated based on customer location and applicable laws. SaaS Revenue Recognition: Adhering to accounting standards for deferring reporting of revenue. Best Security Practices Employ secure payment gateways and encrypted APIs. Scan your SaaS billing application for security vulnerabilities regularly. Implement multi-factor authentication for admin and customer dashboards. How to Select the Best SaaS Billing Solution The best SaaS billing software is based on your business growth model, size, and strategy. Consider the Following Scalability: Does the solution grow with your business? Integration Capabilities: Does it integrate
SaaS Ecommerce: Platforms, Features, Pricing & Business Model Explained The evolution of SaaS ecommerce platforms has changed the way online stores are designed, operated, and grown by businesses. As compared to traditional self-hosted method, Software as a Service (SaaS) ecommerce platforms provide cloud-based technology that is fast, scalable, and affordable. Whether small business enterprise or multi-national company, companies now utilize best SaaS ecommerce software for automating processes, saving cost, and providing improved customer experience. What is SaaS Ecommerce? SaaS ecommerce is software that runs on the cloud and allows companies to create, run, and host web stores without having to deal with backend infrastructure or hosting on the company’s website. SaaS ecommerce differs from open-source ecommerce alternatives that require an enormous amount of technical expertise and server management since custom SaaS ecommerce solutions offer a plug-and-play solution. SaaS ecommerce business model is typically subscription-based where the customers pay an annual or monthly fee to access features, updates, and support on the website. The model provides business enterprises with the cost-per-year or cost-per-month model and eliminate in-house IT overhead. Business enterprises also enjoy the ease of easy scalability as the customers grow because it is cloud-based. How does SaaS Ecommerce work? SaaS ecommerce stores are hosted on the cloud. Sellers own the software, security, updates, and scalability. Sellers host and manage the software, security, updates, and scalability. Clients access their ecommerce dashboards via web browsers where clients’ products, inventories, customers’ orders, and payments are configurable. Ease, scalability, security, and administration in SaaS ecommerce architecture are all offered by: Cloud Hosting & Storage: Offers data security, quick access, and scalability. Security & Compliance Layers: Places itself between cyber assaults and supports global data regulation compliance. Scalable Performance Management: Assists with managing high traffic via sale surges and spikes. Integrated Payment Gateways: Facilitates secure payment with multiple streams of checkout. Third-party App Integrations: Extends more functionality to the platform via extensions and APIs. Ecommerce SaaS websites also contain APIs for customization, templates, and tools through which businesses can tailor the workflow and storefront without extensive coding. Ecommerce SaaS integration of marketing software, CRMs, and ERPs also improves the operational efficiency and customer interaction. Book Your Free Marketing Consultation Key Features of SaaS Ecommerce Platforms User-Friendly Interface: Graphical dashboards, drag-and-drop editors, and intuitive navigation facilitate easy installation and everyday use. Mobile-Responsive Design: Provides seamless shopping experience across all devices, which is a must in today’s mobile-first culture age. Secure Payment Gateways: Offers multi-payment option with built-in compliance (PCI-DSS), fraud protection, and secure checkout process. Inventory Management: Real-time reporting, automated alerts, central product management, and seamless integration with supply chain systems. Scalable Hosting: Holds the burst traffic without giving up on performance, including uptime during holiday offers or flash deals. In-Built Marketing Tools: SEO optimization, email marketing, coupon codes, social integration, and complete analytics dashboards. Third-Party Application Support: Integration with logistics companies, CRMs, ERPs, marketplaces, and business apps. Multi-Channel Selling: Enables selling from your site, online marketplaces like eBay and Amazon, and social commerce storefronts like Facebook and Instagram. Customization & Personalization Features: Theme libraries, personal templates, and API access for the extreme customization. Customer Support & Community Access: 24/7 customer support and access to a users’ community for the sharing of tips and insight. Best SaaS Ecommerce Solutions Shopify: Most appropriate for small startups and SMEs in need of a SaaS ecommerce that is simple to implement but scalable with huge apps and integrations. BigCommerce: Recognized for innovative B2B SaaS ecommerce functionality, robust SEO functionality, and excellent multi-channel selling functionality. Wix Ecommerce: Most suitable for small businesses that seek affordable, tailored SaaS ecommerce with advanced design functionality. Squarespace Commerce: Most suitable for innovative businesses that need contemporary design and user-friendly, built-in marketing functionality. Salesforce Commerce Cloud: Enterprise-class SaaS ecommerce with comprehensive CRM integration and large-scale scalability for global enterprises. Adobe Commerce (Magento SaaS Edition): Offers the might of Magento combined with the ease of SaaS to large enterprises requiring custom solutions. Volusion: Most suitable for those businesses requiring SEO functionality as part of the solution and heavy data analysis. Shift4Shop: Offers a free version with reasonable features, best for extremely small startups with extremely tiny budgets. SaaS Ecommerce Pricing Models SaaS ecommerce pricing is feature, size, and target market-based. Some of the most common models are: Tiered Pricing: Several plans with product limits, feature access, and bandwidth. Per Transaction Fee: Minimal percentage of sales charge in addition to the subscription fee, generally for the likes of Shopify. Flat Monthly Fee: Fixed monthly charges regardless of the level of sales, for those firms that want the expenses to be as stable. Enterprise Custom Plans: For big businesses that require more features, priority support, and custom integrations. Examples of base prices: Shopify Basic: $39/month BigCommerce Standard: $39 per month Wix Business Basic: $27/month Squarespace Commerce Basic: $36/month Salesforce Commerce Cloud: Custom pricing Prices rise with usage, additional ecommerce SaaS features, or items sold, so it is important that businesses compare solutions that fit tomorrow’s and today’s needs. Advantages and Disadvantages of SaaS Commerce Advantages: Low startup cost and constant recurring fees. Easy to install with minimal technical skills needed. Vendor conducts auto-updating, security patches and
SaaS Sales: Strategies, Funnels, Metrics & Best Practices Explained Software as a Service (SaaS) revolutionized the selling and buying of software by businesses. SaaS selling is proactive, relationship customer, subscription, and customer lifetime value-driven as opposed to the traditional software selling model. Regardless of your role, startup leader, sales leader, or career advancement, you have to understand what SaaS selling is and how it works in order to succeed in today’s age of digital disruption. It covers everything about SaaS sales process and strategy to metrics, funnels, and industry best practices. What Is SaaS Sales? Saas Sales is quite simply the resale of a subscription of cloud software to end-user or business clients. It’s different from selling one time perpetual license to software because SaaS sales is actually selling something where there is buying and managing subscribers that pay a fee periodically on a monthly or annual cycle in order to continue accessing a service. The key to SaaS sales is addressing customer requirements with adaptable software solutions—project management software, CRM software, or data analysis software. The SaaS Sales Model Defined The SaaS model of sales will most likely be a subscription model, opting for recurring revenue rather than transactions. The model relies on long-term relationships and success of customers as ways of handling churn. Common SaaS Sales Model Are: Self-Service Model: End users go to the website and sign themselves up (most common on low-dollar SaaS products). Transactional Model: Using a sales organization with medium-dollar transactions using the inside sales technique. Enterprise Model: Long-cycle, high-touch selling by account reps and custom solutions—traditional B2B SaaS selling. Moving on to Understanding the SaaS Sales Funnel The SaaS sales process is the map that guides a prospect to paying a client. There is a customized approach to each step toward maximum conversion. Steps of Most Popular SaaS Sales Process Lead Generation: Generation of potential customers through inbound and outbound marketing. Qualification: Qualifying leads using BANT (Budget, Authority, Need, Timing). Demonstration/Pitch: Customizing your SaaS sales pitch to demonstrate value and alleviate pain for the customer. Negotiation & Closing: Handling objections and closing. Onboarding & Retention: Creating customer delight for long-term retention and cross-sell. An effective SaaS sales process optimizes maximum conversion rate and minimizes the SaaS sales process. SaaS Sales Strategy: How to Win A successful SaaS sales strategy is all about finding customer needs, creating value, and building long-term relationships. Best SaaS Sales Strategies: Value-Based Selling: Highlight the real benefits your software delivers. Solution Selling: Address customers’ tailored pain areas. Consultative Selling: Trust-building as a guide, not a peddler. Free Trials & Freemium Models: Try before buying to allow customers to experiment with your product. Account-Based Marketing (ABM): Match high-value customers with personalized contact (critical in B2B SaaS selling). A successful SaaS sales approach is coordinated with marketing and customer success teams to obtain optimal results. SaaS Lead Generation: Feeding Your Funnel Your sales pipeline will be dry without leads. To explain simply, SaaS lead generation is prospecting and capturing prospects. SaaS Lead Generation Strategies Content Marketing: Webinars, whitepapers, and blogs for creating interest. SEO & Paid Ads: Drive traffic to landing pages. Outbound Prospecting: Cold calls, LinkedIn outreach, and email. Partner & Affiliate Programs: Leverage industry partnerships. Webinars & Product Demos: Interactive demos to engage potential customers. Lead generation fuels your SaaS sales process, keeping you up-to-date on qualified leads to convert. Book Your Free Marketing Consultation SaaS Sales Metrics: What to Track To realize optimum performance and project growth, it is a necessity to measure the right SaaS sales metrics. Must-Have SaaS Sales Metrics Customer Acquisition Cost (CAC): The cost of acquiring a new customer. Customer Lifetime Value (CLTV): Revenue earned by a customer during their lifetime. Monthly Recurring Revenue (MRR): Subscription revenue that recurs in a month. Churn Rate: Clients who’d rather leave percentage. Conversion Rates: To customer at every funnel step. Sales Cycle Length: Average time to close a sale. Qualified Leads Per Month: Quantification of lead generation performance. Tracking these SaaS sales metrics helps to align your sales process and show you where to improve. SaaS Sales Hacks to Generate Maximum Returns These are time-tested SaaS sales hacks, and they will ensure you close more deals and develop stronger relationships: Prioritize the Customer’s ROI Rather Than Features. Present Data-Driven Presentations to Create Customized Presentations. Consistently Follow Up Leads. Invest in CRM and Automation SaaS Sales Platforms. Be Patient, Especially Enterprise Sales. Train and Upskill Your Salespeople Regularly. Collaborate with Customer Success Teams. These optimized SaaS sales tips can work like a game-changer to your conversion rates. SaaS Sales Tools You Should Know Great SaaS sales tools make it easy, enhance communication, and unleash best productivity. Best SaaS Sales Tools: CRM Platforms (Salesforce, HubSpot): Leverage leads and customers. Email Automation (Mailchimp, Outreach): Automated follow-up and prospecting. Analytics Tools (Google Analytics, Tableau): Track performance metrics. Proposal Software (etc., PandaDoc): Create and build proposals. Sales Enablement (Chorus, Gong, etc.): Provides call and meeting insights. SaaS sales software: Automate your sales process. SaaS Sales Commission & Compensation SaaS sales compensation and SaaS sales commission plans differ company size,
SaaS Management: Tools, Strategies, and Best Practices As more and more businesses are utilizing cloud software, SaaS application management is a strategic necessity today. Ranging from a small firm with a few platforms to a gigantic firm with a few hundred subscriptions, well-managed SaaS can offer cost-utility, compliance, security, and optimization of digital assets. With more use of SaaS looming on the horizon, so too is the need for SaaS application management being centralized, such as license usage, renewals, access control, and performance monitoring. This handbook covers it all, from tool and technique through best practice in how to best manage your SaaS environment. What is SaaS Management? SaaS management are the processes and the software employed in monitoring, managing, and optimizing the way an organization is leveraging SaaS applications. It encompasses the whole SaaS lifecycle management from procurement through deployment to metering usage, renewing licenses, and retiring them. An effective SaaS management platform assists businesses in automating workloads, managing user access, identifying idle software applications, and enforcing contract and regulatory compliance for software. It is the foundation of modern IT asset management for SaaS-environment-overloaded organizations. Why SaaS Management Is Necessary Excellent SaaS management offers various business-critical benefits: Cost Savings: Avoid overpaying on unused or underused subscriptions with fine-grained SaaS expense management and license administration. Improved Security: Reduce risk with limited unauthorized use and Shadow IT discovery in SaaS deployments. Regulatory Compliance and Auditing: Ensure data privacy along with software license agreement compliance with SaaS compliance management solutions. Operational Efficiency: Automate IT work and boost productivity through SaaS workflows. As SaaS adoption increases, companies tend to lose subscription control, squander unnecessary spend, and expose sensitive information to risk if not governed centrally and automatically. SaaS Management Key Features SaaS management includes various related activities, discussed below: 1. SaaS Discovery All approved and unapproved SaaS applications used in the organization. 2. Usage Tracking SaaS usage tracking usage offering insights on how frequently users make use of a particular platform and how intensively they make use of it. 3. License & Subscription Management SaaS subscription management and tracking level, seats, renewal date, and entitlements on SaaS license management. 4. SaaS Spend Analysis Reporting total spend, cost per user, and ROI for every application. 5. Access & Role Management Limit access to a single SaaS application for a specific user only, as per SaaS security best practices. 6. Vendor Management Track SaaS vendor management KPIs, SLAs, and compliance documents to monitor healthy supplier relationships. SaaS Management Tools to Measure Some of the most useful tools to measure SaaS management are as follows: 1. Zluri Offers real-time discovery, cost savings optimization, user provisioning, and workflow automation. 2. BetterCloud Automates user lifecycles, secures data, and enforces policy for SaaS apps. 3. Torii Reveals Shadow IT, streamlines spending, and tracks usage with smooth integration. 4. SailPoint SaaS Management Best suited for large organizations with an interest in identity security, compliance, and access governance. 5. Cleanshelf Delivers detailed SaaS license use views and SaaS spend management to finance and IT teams. Each SaaS management tool has unique features, choose as per your business size, compliance needs, and automation level needed. Book Your Free Marketing Consultation Some SaaS Management Strategies In order to build an enhanced SaaS management system, implement practices like consolidating control over SaaS, mandating Automated SaaS workflows, defining procurement and compliance policies, tracking license usage, and auditing applications on a regular basis. These practices bring in higher transparency, reduce costs, improve security, and ease vendor relationships. 1. Consolidate Procurement and Onboarding Make all new SaaS purchases go through IT or procurement for gaining visibility and negotiating leverage. 2. Maintain a SaaS Inventory Maintain an active inventory of all installed SaaS software with vendor and license details. 3. Utilize Role-Based Access Grant SaaS access based on job role. Purge unused accounts regularly to prevent sprawl and expense. 4. Automate Renewals and Offboarding Use SaaS renewal tracking reminders and automatic offboarding of users to prevent orphaned accounts. 5. Encourage Responsible Use Regular review and training of staff around license efficacy and data compliance. Best Sustained SaaS Management Practices To maximize SaaS return on investment and preserve security, organizations must unify SaaS management, track utilization and spending, enforce compliance, automate user onboarding and offboarding, and regularly audit applications. All of these actions hold costs in line, reduce risks, and maximize software performance. 1. Monitor Shadow IT Block and prevent unauthorized software with the use of SaaS discovery tools. Unsupported software is a major security threat. 2. Licenses Review Quarterly Balance active users and licenses. Eliminate duplicate seats or consolidate platforms. 3. SLA and Contract Negotiate Negotiate better price and service levels with usage data from suppliers. 4. IAM Platforms Integrate SaaS apps migrate to identity and access management platforms like Okta or Azure AD for security provisioning. 5. Provide Reporting and Dashboards Implement dashboards to track KPIs like usage of licenses, total spend, app performance, and compliance issues. 6. Ensure Data Residency & Compliance Enforce sanction locations for storing data and ensure all apps comply with standards like GDPR or HIPAA in SaaS management compliance. Future Trends in SaaS Management SaaS ecosystem is evolving at a faster rate, and the emerging technologies are providing the next generation of optimization by AI-powered optimization, next-generation SaaS security posture management, unified IT asset and SaaS management, and automated workflows to drive the future. These technologies are designed to enable cost management, security, and operational efficiency for the business. 1. AI-Powered Insights License forecasting, anomaly detection, and usage recommendations will be enhanced by AI capabilities in logistics, enabling smarter decision-making and increased operational efficiency across the supply chain. 2. Tighter Security Integration More sophisticated SaaS security best practices and security orchestration platform integrations will be anticipated. 3. Decentralized IT Models Since business units buy their hardware, aggregated SaaS visibility will be worth more. 4. Increasing Regulation Compliance There will be more controls on SaaS platforms
SaaS Logistics: Smart Supply Chain Management to Cloud Solutions Technology is revolutionizing business company usage of supply chain management, and logistics are being remapped. The software used for managing logistics has evolved a great deal from old-school on-premises models to agile, cloud-based models. The transformation allows companies to achieve ultimate efficiency, simplicity, and control over operations. SaaS supply chain management allows inexpensive and adaptive solutions to be utilized by organizations of all sizes. Cloud logistics solutions allow organizations to relish real-time data, automate operations, and improve the delivery process without major IT investment. What is SaaS Logistics? SaaS logistics refers to cloud-based software utilized to handle logistics and supply chain functions. In contrast to conventional systems, the software is web-hosted and subscription-based. Among them are transport management system (TMS) software, warehouse management SaaS software, and fleet management SaaS software. These are cloud-based software which enable firms to manage everything from inventory control to delivery without laying out money for costly hardware or software licenses. SaaS logistics and shipping guarantees harmonious integration of supply chain procedures, focusing on efficiency and ongoing monitoring. Logistics tracking software provides real-time monitoring of shipments by companies, resulting in better decision-making and customer satisfaction. SaaS Logistics Software Key Advantages Cloud logistics software enjoys the following benefits compared to traditional systems: Cost Savings: No infrastructure cost for capital and assurance of subscription fees. Scalability: Cloud logistics software expands with your expanding business. Accessibility: Perform control operations wherever, whenever you want cloud connectivity. Real-Time Information: Your real-time logistics tracking software provides real-time delivery and stock details. Integration: Tight integration with other company systems, enabling data transfer between platforms smoothly. These are the features that make SaaS for supply chain management the correct choice for companies wishing to streamline operations and lower overheads. Key Features of SaaS Logistics Platforms Solution-specific solutions by emerging logistics SaaS solution vendors address unique needs. Most critical capabilities are: Transport Management System (TMS): Combines planning, execution, and tracking of loads to accomplish optimal route delivery and cost savings. Warehouse Management SaaS: Offers order processing, storage administration, and inventory management functionality. Fleet Management SaaS: Monitors vehicle usage, upkeep, and driver performance to accomplish maximum delivery efficiency. Last Mile Delivery Software: Designed for last-mile delivery optimization to enable on-time order fulfillment. Order Fulfillment Software: Order processing, packaging, and shipping are automated to automate supply chain processes. They are cloud-based, analytics-AI-powered solutions. Advantages of SaaS in Supply Chain Management Supply chain management implementation by SaaS builds operational advantages: Enhanced Visibility: Cloud logistics software allows a single point of access to data and enhances supply chain activities. Enhanced Efficiency: Automated logistics elements of logistics automation platform solutions minimize human error and intervention. Enhanced Decision-Making: Real-time information through real-time logistics tracking software allows managers to make more informed decisions. Less Cost: Pay-as-you-go models guarantee efficient budgets. Businesses that use SaaS to ship and logistically operate become more competitive by offering better customer service and automated transactions. Book Your Free Marketing Consultation Application of SaaS in Logistics Logistics platforms based on SaaS provide support for different segments of the supply chain: E-commerce: Order fulfillment software and last-mile delivery software are used by business firms to ship on time and monitor customer orders. Freight Companies: SaaS freight management solutions enable them to route plan and load optimize. Retail Chains: They use SaaS to control the optimal levels of inventory and avoid shrinkage. Distribution Centers: Take advantage of warehouse management SaaS, which controls automated picking, packing, and storage operations. Fleet Operators: Take advantage of fleet management SaaS, which controls vehicle performance and driver behavior. Below are some of the avenues through which various industries benefit from SaaS in supply chain optimization. Challenges and Considerations Despite being beneficial, SaaS logistics also has challenges: Data Security: Use of cloud services comes with concerns about sensitive information. Difficulty in Integration: Incorporating logistics management software into current business systems is challenging. Vendor Reliability: Not every company that offers SaaS logistics offers the same service or uptime guarantee. Limitations of Customization: Certain cloud-based logistics software has little room to customize compared to on-premise systems. These are things one must learn well in advance before deciding on a platform to automate logistics for your enterprise. Selecting the Proper SaaS Logistics Platform When selecting a SaaS platform, follow these: Features & Functionality: Make sure the platform has the type of transport management system (TMS), warehouse management SaaS, and order fulfillment software relevant for your business. Scalability: Make sure cloud logistics solutions scale up to support your organization’s requirements. Integration: The platform should integrate well with your current ERP or CRM platforms. Vendor Reputation: Check customer reviews, uptime record, and service quality of logistics SaaS providers. AI & Automation Features: Logistics SaaS solutions with AI capabilities provide predictive analysis and automation of decision-making. Smart choice will get your shipping and logistics SaaS investment yielding returns in the long term. SaaS Logistics Future The future of SaaS logistics is favorable with recent advancements such as AI, IoT, and blockchain. AI in Logistics SaaS: Artificial Intelligence will further transform demand forecasting, route optimization, and risk management. Logistics Automation Platform: Automation will make supply chain operations smooth, from tracking stocks to automated delivery systems. Real-Time Logistics Tracking Software: IoT will enable companies with even better tracking and predictive
SaaS Accounting: The Comprehensive Guide to Revenue, Billing & Compliance SaaS businesses have unique business and financial models that require unique accounting methods. Business Schools need to cover this: SaaS businesses versus product businesses. When compared with product businesses, issues related to recurring revenues, long-term customer relationships, and complex compliance issues are uniquely relevant to SaaS businesses. The answer to the question What is SaaS accounting? is particularly important for accounting and finance teams that need to run operations, maintain compliance, and make decisions based on facts. This guide covers everything from the unique accounting for SaaS companies to revenue recognition, billing types, financial statements, metrics, and more automated compliance and forecasting tools. What is SaaS? SaaS accounting refers to the contribution of the financial administration and bookkeeping of the Software as a Service (SaaS) organizations. SaaS companies have recurring revenue which comes in form of subscriptions unlike in traditional businesses meaning it has special revenue recognitions, tracking of deferred income as well as specialized metrics which include Monthly Recurring Revenue (MRR), Annual Recurring Revenue (ARR), and Customer Lifetime Value (CLV). SaaS accounting estimates within tolerance in order to provide good forecasts, reporting to investors, and strategy. It usually employs cloud-based accounting systems that mainly support subscription billing, CRMs and payment gateway services and the software makes the process of financial reporting for SaaS business automated and scalable. Unique Challenges in SaaS Accounting Accounting challenges in SaaS are due to the subscription model. In contrast to retail, the revenue cannot be recognized upfront. Rather, it must be recognized throughout a customer’s subscription. Accrual accounting is required for SaaS. Accounting challenges of importance in SaaS include: Servicing multi-period contracts Accrued revenue management in SaaS Compliance with SaaS rules under ASC 606 Recurring revenue monthly (MRR) and annually (ARR) calculation Convergence of subscription billing accounting systems In addition, SaaS companies must address issues like the management of cash flow SaaS where advance payments skew near-term liquidity. Principles of Substantive SaaS Accounting SaaS accounting is founded on principles that ensure financial reporting is accurate and regulatory compliant. They are: 1. Accrual Accounting Accrual accounting for saas retains revenue and expense on the books whenever earned or incurred but not when cash is paid. This method of accounting provides a better picture of the real financial position of a company. 2. Revenue Deferral Deferred revenue for SaaS means payment made in advance of services completion. In a customer paying annual plan upfront, one-twelfth of the revenue is recorded each month. 3. Revenue Recognition Compliance With ASC 606 SaaS compliance, businesses must recognize revenue at satisfaction of performance obligations and not when cash is received. Adhering to the standard helps align finances with economic activity. These foundations lie at the center of accounting integrity for SaaS businesses and promote transparency for stakeholders and regulators. Book Your Free Marketing Consultation Revenue Recognition in SaaS SaaS revenue recognition is based on ASC 606, an internationally accepted standard manual. ASC 606 requires SaaS companies: Identify a customer contract Define performance obligations Determine the transaction price Allocate price to obligations Recognize revenue on fulfillment of obligation This is especially crucial for tiered-pricing or multi-service businesses. For example, if a SaaS business offers onboarding support along with the software license, it must break and defer the revenue accordingly. Good SaaS revenue recognition keeps companies in compliance and to make sound financial choices. Some automate it using saas accounting software. SaaS Billing Models Subscription accounting billing adds one more complexity to SaaS operations. Common billing cases are: Flat-rate billing: One flat rate for all usage. Tiered pricing: Multiple plans based on features or levels of usage. Usage-based billing: Charge on actual usage (e.g., per API call). Hybrid billing: Combination of fixed fees and usage-based fees. Every model impacts revenue forecasting SaaS, customer turnover, and revenue accounting. Usage models, for instance, will require estimates and patches on every billing cycle. Business-built billing systems not only bring revenue precision but also improve cash flow management SaaS, especially for high-growth companies. SaaS Financial Reporting & Metrics Financial reporting for SaaS businesses is more than balance sheets and income statements. SaaS companies use performance measures almost solely in terms of operating metrics. Saas financial metrics of interest include: Monthly Recurring Revenue (MRR): Measures recurring revenue earned in a month. Annual Recurring Revenue (ARR): Annualized version of MRR. Churn Rate: Number of customers or revenue lost over some time. Customer Lifetime Value (CLTV) Customer Acquisition Cost (CAC) Monitoring churn rate and revenue impact is especially crucial. Inordinate churn can cripple expansion regardless of whether acquisition is robust. Monitoring these saas financial metrics allows companies to act pre-emptively and decide to optimize price or product strategy. Reporting also allows revenue projecting SaaS, allowing leaders to prepare for hiring, growth, or fundraises. SaaS Accounting Tools & Software With the sophistication of subscription billing and compliance, companies make wide use of master saas accounting software. These solutions aid: Subscription billing accounting ASC 606 SaaS compliance Deferred revenue schedules Consolidated financial reporting MRR/ARR dashboards A few of the popular solutions are: QuickBooks with SaaS add-ons Xero with subscription plug-ins Chargebee and Recurly for automated billing NetSuite for enterprise-level reporting Precise saas accounting software can automate processes, reduce errors, and enable your staff to spend more time on strategic goals rather than manual data entry. Best Practices for