VOB in Medical Billing: What It Means and Why It Matters Healthcare billing gives many providers headaches. Getting paid for services shouldn’t be this complicated, but insurance companies make it tough. Verification of benefits in healthcare stands out as one step that can save practices from major problems down the road. Insurance plans keep getting more confusing each year. What used to be simple coverage now involves multiple layers of approvals, different cost levels, and endless rules. Smart healthcare providers check patient benefits before starting any treatment. This simple step prevents nasty surprises that can hurt both the practice and patients. What is VOB (Verification of Benefits)? VOB means checking what a patient’s insurance will pay before you treat them. The VOB process in medical billing involves contacting insurance companies or using online tools to find out coverage details. Think of it like calling ahead to make sure a restaurant takes your credit card before you order dinner. This goes way beyond just asking “Do you have insurance?” Real verification digs into the specifics. How much does the patient owe upfront? What treatments does their plan cover? Do they need special permission for certain procedures? These details matter when it comes to getting paid. Most practices now use computer systems that connect directly to insurance databases. These tools give quick answers about basic coverage. But computers miss things sometimes. The tricky cases still need a human touch – actual phone calls to insurance reps who can explain the fine print. Key Components Verified During VOB A solid VOB checklist for insurance covers several must-have items. Active coverage comes first. Just because someone has an insurance card doesn’t mean their plan is current. People lose coverage when they miss premium payments or change jobs. Deductible amounts need checking too. This is how much patients pay out of pocket before insurance kicks in. Some plans have different deductibles for office visits versus hospital stays. Others reset every year in January. Getting this wrong means surprises for everyone. Copay and coinsurance details matter for every visit. Copays are flat fees like $25 for office visits. Coinsurance is percentage-based – maybe the patient pays 20% while insurance covers 80%. These amounts change based on whether you’re in their network or not. Coverage limits and exclusions trip up many providers. Insurance companies love to exclude certain treatments or limit visit numbers. Mental health might have different rules from physical therapy. Knowing these limits upfront saves headaches later. Network status affects everything else. In-network providers get better rates and easier approvals. Out-of-network care costs patients more and creates extra paperwork. Always confirm your network status for each patient’s specific plan. Prior authorization requirements can kill claims if missed. Many procedures need advanced approval from insurance companies. Skip this step, and they won’t pay anything, even for covered services. Why is VOB important in Medical Billing? The importance of VOB in revenue cycle management shows up in practice in bank accounts. Providers who skip verification steps see more claim denials, slower payments, and frustrated patients. Those who verify benefits upfront run smoother operations and collect money faster. Patient relationships improve dramatically when cost discussions happen before treatment. Nobody likes surprise medical bills. When you can tell patients their expected costs upfront, they appreciate the transparency. This builds trust and reduces payment disputes. Insurance coverage verification helps practices follow all the insurance company rules. Each insurer has different requirements for documentation, approvals, and billing procedures. Understanding these rules beforehand keeps claims from getting rejected for technical reasons. Bad debt drops significantly when practices collect money at service time. If you know the patient owes a $50 copay, collect it during the visit. Chasing payments later through bills and collection calls costs more time and money than upfront collection. Book Your Free Marketing Consultation How does the VOB Process work? How to perform VOB starts when patients schedule appointments. Office staff should gather complete insurance information, not when patients arrive for treatment. This includes primary insurance, secondary coverage if they have it, and current policy details. Electronic checking usually comes first. Medical insurance VOB systems connect to major insurance databases and pull coverage information instantly. These tools work well for basic verification but sometimes miss important details about specific benefits or restrictions. Phone verification fills in the gaps. Calling insurance companies directly takes more time but provides detailed answers about complex coverage questions. Keep good notes about who you talked to and what they said. Insurance reps sometimes give wrong information, so documentation protects your practice. VOB before treatment timing matters for different service types. Routine appointments need verification a few days ahead. This gives time to handle any problems discovered. Emergencies require immediate verification, but some checking is better than none. VOB for outpatient services tends to be simpler than inpatient procedures. Outpatient care usually involves fewer approvals and less complex billing. But don’t skip the basic steps just because it seems routine. Regular re-verification helps with ongoing treatments. Insurance benefits can change monthly. Annual deductibles reset in January. Coverage that worked last month might not work this month, especially for patients getting regular care. Common Challenges in VOB Common VOB errors often start with bad patient information. People carry old insurance cards, forget about secondary coverage, or don’t understand their benefits. Starting with wrong information leads to wrong verification results. Insurance company systems create their problems. Computer databases don’t always match current coverage details. Representatives sometimes give conflicting information about the same patient. These inconsistencies make verification frustrating and time-consuming. VOB denial reasons include missing authorizations, using the wrong procedure codes, and exceeding benefit limits. Many practices see patterns in their denials that could be prevented with better upfront verification. Staff training gaps cause expensive mistakes. If team members don’t know proper verification procedures, they skip important steps or document things incorrectly. Regular training updates help prevent these costly errors. Busy practices sometimes rush through verification to save time. This penny-wise, pound-foolish approach leads to bigger
EOR in Medical Billing: Meaning, Process, Denials & Appeal Guide In the complex medical billing arena, coders, billing personnel, and medical providers should be aware of payment processes. Among the essential documents to this process is the Explanation of Review, or EOR. Although often confused with other documents like EOBs or remittance advice, the EOR has a different purpose in ensuring proper claim processing, denial, and appeal. This article will walk you step by step through everything you wish to know about EOR, from what it is and how to interpret it to denials and appeals. What is Medical Billing EOR? The EOR meaning in insurance definition is the explanation of review medical billing, which is a third-party payer’s or insurance company’s notice that describes how a medical claim EOR was processed. It can contain details like disallowed charges, allowed charges, payment, and the reason for any adjustments or denials. Most providers ask, What is EOR in medical billing? In short, it is a description of the insurer or third-party administrator’s decision on reviewing a healthcare claim submitted. It allows providers to be aware of reimbursement status and if any follow-up action, like an appeal, is needed. EOR Components A EOR document in healthcare typically includes: Patient details and reference number for the claim Service dates and CPT/HCPCS codes Billed charges and allowed amounts Denial codes and explanations Amount paid (if any) Payer comments Reasons or explanations for adjustments These components help billing staff balance payments and detect anomalies. It is necessary to understand EOR descriptions and codes to accurately interpret the document. EOR Process: A Step-by-Step Guide The payor EOR process begins when a healthcare provider initiates a claim after providing medical services. The following describes how it unfolds: Claim Submission: The physician submits an accurate bill to the payer. Claim Review: The payer EOR process reviews the claim for medical necessity, coding compliance, and coverage under the plan. EOR Generation: Upon review, the payer issues an EOR stating how the claim has been processed and how much is going to be paid. Claim Payment/Adjustment: Pay is released according to the EOR, or adjustments are made. Provider Review: The provider verifies the EOR to confirm accuracy in payment or to identify inconsistencies. Follow-up: Upon denial or error, the provider can initiate an EOR appeal process. The entire process is crucial for timely payments and precise finances in health care facilities. Common Reasons for Denials in EOR There are a number of EOR denial reasons that can occur and ultimately impact the payment. Some of the most frequent include Incorrect or inadequate patient information Incorrect CPT or diagnosis codes Services that are not covered by the patient’s plan Not pre-authorizing Missing documentation or clinical notes Billing the same service twice Service deemed medically unnecessary When these kinds of issues arise, the payer will include denial codes and concise explanations in the EOR to help providers understand the reasons for non-payment or partial payment determination. Book Your Free Marketing Consultation How to Read and Understand an EOR For billing teams and providers, it is very important to be able to read EOR so that claim reconciliation and revenue cycle can be accurately managed. An EOR can appear technical, but demystifying it makes a difference. Check Patient and Claim Info: Make sure it is what was submitted. Compare Charged vs. Allowed: Look at what insurance considers reasonable. Review Denial or Adjustment Codes: Each code is a reason for denial or adjustment. These are important to know. Analyze Paid Amounts: Look at how much was paid and determine whether it meets your expectations. Search for Explanatory Notes: The majority of EORs have narrative comments or remarks that provide context. Healthcare professionals often equate the EOR to the EOB. During the EOR vs EOB controversy, notice that even though both are payer-issued documents, an EOB is patient-facing, while an EOR is provider-facing with more billing-related information. Appeal Process Following an EOR Denial When a provider disagrees with an EOR outcome, the secondary action is the appeal process of an EOR. This includes filing an appeal to the insurer, accompanied by documents that refute the denial or adjustment. Steps in the Appeal Process: Careful Reading of the EOR: Check the denial code and reason. Gathering of Documentation: These include medical history, physician documentation, or claims reprocessing. Prepare a Legible Appeal Letter: Fill in patient and claim data, state how the denial is incorrect, and attach proof. Mail to the Correct Department: Ensure it’s sent to the payer’s appeals department by the time limit. Appeals typically result in payment reversals, especially if aided by proper documentation. Knowing how to operate claim adjustments in EOR as well, some are fixed, and others reverse on appeal, is also essential. Tips for Successful EOR Management Successful management of EOR is key to revenue leakage containment. The following are some essential tips: Train Billing Teams: Make them masters at reading EOR on the bill and familiar with denial codes. Utilize Practice Management Software: These programs assist with matching claims, EORs, and payments faster. Develop Standardized Appeal Templates: Saves time when appealing denials. Track Trends: If particular services are constantly denied, this can assist in identifying underlying issues. Deal with Payers: Develop relationships and request clarifications if an EOR is ambiguous. For complex or high-volume claims, practitioners frequently outsource billing to third-party EORs in billing specialists to handle the nuances of payer communication and appeals. Conclusion EORs are an integral part of the medical billing process. They serve as a guide to learning how claims become audited, adjusted, and reimbursed by insurance. Like EOR vs remittance advice but with specific details critical in revenue cycle management, the EOR is an important tool in the insurance billing process. Understanding the difference between EOR and remittance advice is
EOB in Medical Billing: How to Read and Understand Your Explanation of Benefits When your insurance is billed and you receive your health care, in the end, you will be receiving your Explanation of Benefits, better known as your EOB. The letter is typically confusingly mistaken for being a bill, but this precious piece of paper is used for a completely different purpose. Explanation of benefits in medical billing provides the patient and provider an easy-to-read breakdown of the way in which the insurance company has processed the claim, the amount paid by them, and what the patient will pay. But because it is so significant, most patients will forget the EOB or never even comprehend it, subsequently resulting in confusion, overpayment, or missed problems. This tutorial will assist you in knowing precisely what the EOB is, what it means, and how you might employ it for your benefit. What is an EOB? EOB is an explanation of benefits in the context of health care, and it is an appropriate notice from your insurer describing how a health claim was processed. It will contain important information like what kind of service you received, what the healthcare provider billed you for, what your insurance paid out, and what remaining amount you are supposed to pay. This is not a bill. But it’s worth knowing and reading because it affects your overall healthcare cost and can signify whether action is required by you, such as paying a balance or contesting a denied claim. The Difference Between EOB and a Medical Bill One of the most frequent patient misconceptions is finding the difference between the EOB and the medical bill. Even though they look the same and are both costs of healthcare, they have very different purposes. The EOB is yours from your insurance company. It is a report that explains how they handled the claim that was filed by your healthcare provider. The medical bill, however, is your hospital, clinic, or doctor’s request to pay. The two can be compared to ensure accuracy, ensure insurance pays, and find billing errors. How to Read an EOB Fewer than half of patients aren’t certain what to do with an EOB, and that creates an opportunity for billing errors or claims denials to fall through the cracks. A standard EOB has a few key items: Patient Information: Your name and insurance ID number. Provider Information: Name and address of the health care provider who rendered the services. Description of Service: Medical service rendered and date of treatment. Amount Billed: The provider charges billed to the insurer for payment. Allowed Amount: The insurer’s ruling of what was reasonable for the service. Paid Amount: What your insurer paid to the provider. Patient Responsibility: Any amount you pay out-of-pocket, e.g., deductibles, coinsurance, or not covered services. Remark Codes: Usually abbreviated and defined at the end of the document, these stipulate adjustments or denials. Familiarity with these areas ensures that you know where your funds are being spent and what you can expect in the way of financial responsibilities. Example EOB Medical Billing – Without the Confusion In order to understand an example of a sample EOB medical billing form, it is simpler to think in terms of a specific example. Suppose you had a medical test that cost you $300. Your insurance company can cover just $200 as billable under your policy, reimburse $150 of it, and charge you the rest of $50. While this is not indicated in a table here, the EOB would mention each of these items briefly. Going over these figures and comparing them to your doctor’s bill allows you to detect discrepancies early. This way, your payment responsibility is accurate and your insurance coverage is working as intended. The Role of EOB in Claim Processing It is important that the providers as well as the patients know the role of EOB in claim processing. To the insurance providers, the EOB can serve as a communication channel to facilitate transparency. To the patients, it provides the scope to check the claim processing and detect errors or omissions. It also assists medical offices in reconciling claims against payments and posting patient accounts correctly. Incomplete or inaccurate EOBs can disrupt billing cycles or overcharge patients. Book Your Free Marketing Consultation Justification for EOB Denials Your EOB sometimes indicates a service as denied or partly paid. Such reasons for EOB denial are justified in the form of codes or short descriptions on the EOB. Some such common causes are: The service was not covered under your plan of insurance. The provider did not have prior authorization. The claim was late in submission. The data were incorrect or insufficient. The service was not deemed medically necessary. When your EOB denies, you need to follow up. Sometimes a call can get things sorted out quickly, or you are filing a protest. How EOB Affects Medical Billing It is important to understand how EOB affects medical billing is important. The EOB indicates the amount your insurer has paid and the balance, if any, that still needs to be paid by you. Providers use the information in the EOB to update your account and provide accurate bills. If you don’t read or understand your EOB, you could overpay or be charged for already-covered services. Providers may also fail to bill you for legitimate patient responsibilities, resulting in surprise balances or collections later on. EOB Codes and Descriptions Explained Most EOBs include different short codes that are difficult to decipher at first glance. These EOB codes and descriptions are employed by insurance firms as fast reference points for payment, adjustment, or denial explanations. For example, a code can indicate the procedure was only partly reimbursed, or a repeat claim. A majority of codes also include their descriptions in the back or bottom of the EOB. It is well worth the effort to study these codes, especially if you
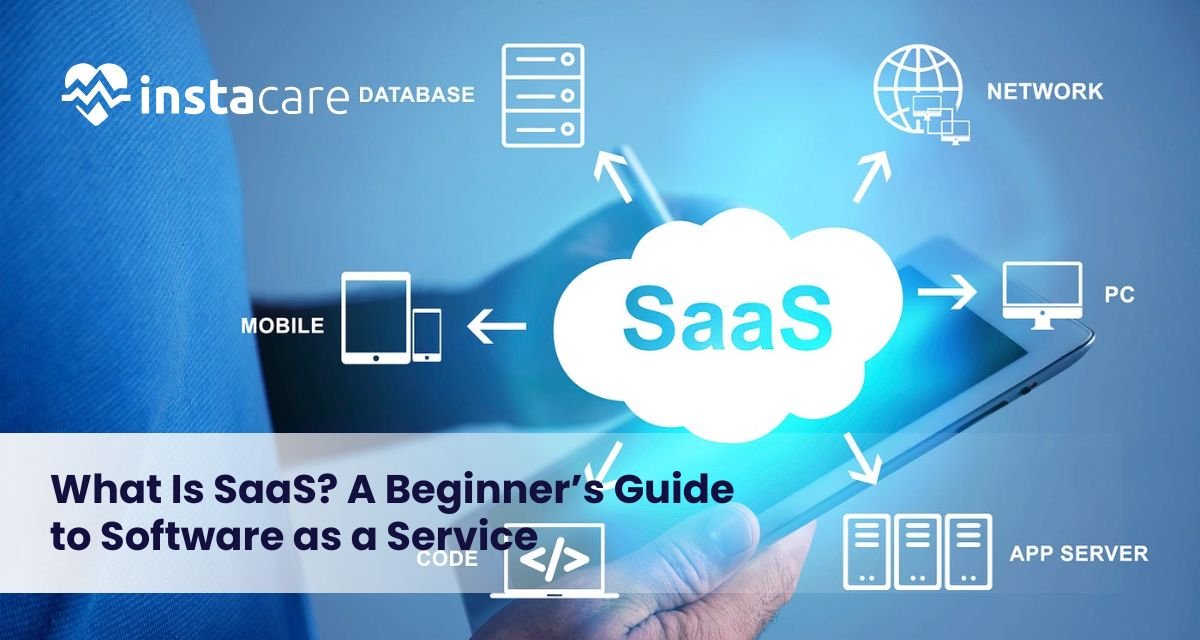
What Is SaaS? A Beginner’s Guide to Software as a Service Ever since the beginning of the age of computers and digital technology, companies and individuals have depended increasingly on software to carry out day-to-day tasks, communicate with each other, keep information stored, and perform processes automatically. Some of the most significant advances in history have been the invention of cloud-based software, that is, Software as a Service (SaaS). Precisely what is SaaS, anyway? How are folks using it, and why is it so globally popular among so many different types of industries? This beginner’s guide contains everything you ever wanted to learn about SaaS from the way it works to its advantages, examples, and problems prior to implementation. What Is SaaS? SaaS meaning is “Software as a Service,” which is an on-demand delivery model for software where a third-party company owns the software and hosts it on the internet to customers. Rather than installing and maintaining software on individual computers or internal servers, customers can access web browser-based SaaS applications on a pay-per-use basis. The SaaS definition can be employed to articulate a wide variety of software solutions, from productivity suites like Google Workspace to customer relationship management (CRM) solutions like Salesforce. Unlike traditional software, which has to be installed physically and updated periodically, SaaS provides perpetual access, ongoing updates, and minimal setup. History of SaaS traces back to the 1960s when mainframe computing rendered sharing of software on use inevitable. The modern SaaS model which started gaining momentum in the course of the late 90s was pioneered by Salesforce through offering web-based software. SaaS has since become a ubiquitous application structure of business establishments of any size implementing software. How Does SaaS Work? To learn about SaaS, consider renting software instead of purchasing it. SaaS applications are stored on the provider’s servers. The provider does all the work: hardware, software updates, security, and infrastructure. Users just log in over the web to access the software. The SaaS model is usually accompanied by recurring fees, annual or monthly. Both the user and producer benefit from the model. Producers get stable revenue, while users avoid front-end expenses and pay when they use. One of the advantages of SaaS includes: Multi-tenancy: Various users share one infrastructure but maintain their data segregated. Automatic updates: Features and fixes are provided without involving users. Accessibility: Individuals can utilize software from anywhere they are accessing the internet. Scalability: Simple to scale up or down usage depending on the requirement. Advantages of SaaS Advantages of SaaS are many and have made it present in nearly every sector. Below are the main advantages: Cost-Efficiency: No hardware or software acquisition cost. There is a subscription fee, which spreads the cost over time. Ease of Use: The majority of SaaS solutions are easy to use and don’t demand technical expertise to become operational. Availability: Clients can access software through any device that is networked, which allows working remotely and communicating. Scalability: The companies are easily able to scale up and down with no concern for infrastructure. Security: The best security features are readily available, including encryption, backup, and compliance certification of the SaaS vendors. Automatic Updates: The security patch and updates are automatically applied. Integration: SaaS applications will typically integrate with other company software to enable process streamlining. There are SaaS pros and cons, but even with those pros. Some of the cons include the absence of control over customization, reliance on internet connections, and vulnerability to data security breaches if left unattended. Book Your Free Marketing Consultation Common Use Cases of SaaS SaaS applications today touch nearly all personal and business operations. Below are some of the most utilized SaaS businesses and software: ● Collaboration & Communication Remote work necessities include tools such as Slack, Zoom, and Microsoft Teams. ● Customer Relationship Management (CRM) Salesforce, HubSpot, and Zoho CRM are programs that manage company sales pipelines and customer relationships, similar to how Clinic Management Software helps healthcare providers streamline patient interactions, appointments, and administrative workflows. ● Accounting & Finance Easy-to-use bookkeeping software is offered by cloud-based solutions for small and medium-sized businesses, such as QuickBooks or Xero. ● Project Management Asana, Trello, and Monday.com make task management and collaboration with a team extremely simple. ● Marketing Automation ActiveCampaign and Mailchimp make email marketing, email segmentation, and lead nurturing easy. ● E-Commerce Both Shopify and BigCommerce allow businesses to create storefronts online without being experts in web development. ● Human Resources BambooHR and Gusto help in automating Human Resources services, such as onboarding, payroll, and benefits services. ● File Storage & Sharing Google Drive and Dropbox enable one to save business and personal files in the cloud. SaaS in healthcare is fast developing in the niche markets with electronic health record (EHR) systems, telemedicine software, and patient scheduling applications Key Considerations Before Choosing a SaaS Product There are numerous benefits of SaaS, but choosing an appropriate one requires vigilant consideration. The following are key things to consider: Data Security and Privacy: Consider how the SaaS provider approaches data backup, data security, and regulatory compliance (e.g., GDPR, HIPAA.). Pricing Model: Find out how much it will cost in total: subscription fee, fee per extra user, license to watch. Integration Capabilities: Ensure that the SaaS product fits into your existing equipment and infrastructure by not causing too much of a wrench in your operations. Service Level Agreements (SLAs): SLAs have guarantees of uptimes, support response, and support that is important to the mission-critical applications. Scalability: Go with a platform that scales along with your business and has scalable pricing plans. SaaS vs PaaS vs IaaS SaaS is one of the three basic models of the long list of cloud computing. The other three models are PaaS and IaaS models. SaaS (Software as a Service): pre-installed software over the web (e.g., Gmail, Dropbox). PaaS (Platform
Edge Computing in Healthcare: Transforming Real-Time Patient Care Modern healthcare depends heavily on digital technology to propel patient care and process automation. Of all those technologies, edge computing is arguably the most important. Edge computing processes data at or near its origin, near the patient or medical device, instead of having all of it routed to distant cloud servers. This edge computing enables low-latency healthcare applications, which are critical in real-time patient monitoring and remote patient monitoring systems. Healthcare providers can enable faster, safer, and more reliable data processing at the edge through the assistance of edge computing, with direct effects on patient outcomes. With growing numbers of medical IoT devices and connected health platforms, healthcare ecosystems are rapidly becoming more complex and edge computing offers solutions to volume, speed, and data privacy. This article here explains what edge computing is, why it is so important in the context of healthcare, its key applications, benefits, and upcoming trends shaping the future of healthcare delivery. What is Edge Computing? Edge computing is a distributed IT platform where the processing happens at or near the edge where the data is created instead of shipping it to a remote data center or cloud. “Edge” refers to the physical site at the network edge, like a ward in a hospital, a wearable, or an off-site clinic. In healthcare, edge computing enables processing at the edge, on nearby devices or intelligent devices, and carries computation to patients, introducing less latency for data transmission required by time-sensitive healthcare processes. The technology enables applications with secure real-time health data that can make medical decisions feasible in a timely and reliable manner. In contrast to bandwidth and latency-constrained traditional cloud computing, edge computing offers an appealing and real-time processing of immense amounts of health data that are generated by internet-connected devices. Applications of Edge Computing to Healthcare Healthcare is uniquely suited to adopt edge computing because of the demands of fast data processing and privacy safeguarding. Edge computing has a variety of its most important applications in the healthcare sector: Real-time monitoring of patients: Sensors and wearables monitor patients’ vital signs in real-time. Real-time analysis is done by edge computing, allowing healthcare providers to respond early to dramatic changes. Security and privacy of data: Personal health data is processed locally, reducing the likelihood of transmission breach. Conservation of bandwidth: No data is transmitted to the cloud; only processed or necessary data is sent, defragmenting the network. Better decision-making: Real-time analysis at the edge device enables timely, informed clinical decisions. Rural and remote healthcare: Edge computing ensures effective delivery of health even in areas with sparse or patchy internet coverage. As 5G and edge in healthcare continue to expand, data reliability and speed are enhanced, enabling more sophisticated healthcare applications. Major Applications of Edge Computing in Healthcare Edge computing enables different healthcare innovations and solutions: Remote patient monitoring systems: Medical devices that track important indicators like heart rate, blood glucose, and oxygen level remotely process them locally to trigger alarms on abnormalities. It is vital for the management of chronic conditions as well as post-operative monitoring. Edge AI in healthcare: Edge AI in healthcare algorithms to support early diagnosis, personalized treatment plans, and predictive analysis without ever relying on the cloud. Edge analytics in healthcare: Healthcare organizations utilize edge analytics in patient care to track machine performance, predict failures, and streamline processes. Medical edge devices: Intelligent medical devices such as infusion pumps, ventilators, and imaging scanners use edge computing to work at their best and in a secure manner. Processing data at the edge: Processing data close to the patient location, healthcare workers eliminate delays, optimizing response in the case of an emergency. Medical IoT and edge computing: Connected healthcare equipment produces continuous, fluid streams of data, processed by edge computing to enable real-time monitoring and control. Edge computing use cases in hospitals: From intelligent operating rooms to patient flow management automation, edge computing enhances hospital workflows. Book Free Demo Edge Computing in Healthcare Benefits Healthcare acceptance of edge computing is followed by an array of benefits: Decreased latency: Faster processing enables rapid, time-sensitive, critical decisions in emergency and critical-care situations. Enhanced data security: Local processing lowers exposure to cyber attacks and enables easy compliance with privacy regulations like HIPAA. Enhanced patient care: Real-time observations and rapid data analysis facilitate on-time intervention and enhanced treatment protocols. Reduced costs: Reduced data transmission and cloud storage requirements save healthcare centers on IT expenses. Business continuity: Edge devices can operate in isolation during network downtime, enabling uninterrupted healthcare services. Smart healthcare infrastructure support: Connecting with 5G networks increases data speed and dependability, facilitating pioneering health technology. Health organizations embracing the edge computing benefits in healthcare realize increased efficiency, patient satisfaction, and data security compliance. Edge Computing Innovations and Future Trends The future of healthcare edge devices is auspicious, with loads of innovation on the way: 5G adoption: 5G network rollout adds edge computing with low-latency healthcare solutions and super-high-speed connectivity critical to telemedicine and real-time health monitoring applications. Enhance edge AI: Edge device AI applications will continue to evolve and get better at enhancing diagnostics, patient risk stratification, and individualized care. Healthcare edge device innovation: Networked medical devices and intelligent wearables will fuel edge data generation and processing. Improved security: As more organizations move to the edge, encryption and strong defense mechanisms for protecting real-time health information will be critical. Cloud-edge hybrid models: Blending the elasticity of the cloud
ChatGPT vs Healthcare-Specific AI: Which Model Helps Medical Software More? AI is making a positive impact on healthcare by boosting the performance and accuracy of medical software. AI tools today can be classified into two categories: those designed for broad use, such as ChatGPT, and those for use in healthcare. Discussions around ChatGPT vs Healthcare-Specific AI point out some important factors, for example, adaptability, compliance, and expertise in healthcare. Medical institutions and developers must decide on the model that best meets their planned improvements in diagnostics, managing tasks, or patient communication. This article compares ChatGPT with custom healthcare AI systems, detailing the main differences, highlighted strong points, potential challenges and their applications in software used in healthcare. Understanding ChatGPT and Healthcare-Specific AI? ChatGPT ChatGPT is a language model that OpenAI has developed for general use. It can handle human-style communication and is often applied for creating content, helping with customer support, and responding to basic questions. One use of ChatGPT in medical software is to assist in making simpler patient notes, listing instructions for patients, and making it easier to communicate with them. AI Designed for Healthcare Alternatively, AI designed for healthcare is prepared using the rules and standards found in medical data. In most cases, these models are tied to EHRs, diagnostic tools, and how clinicians work in their specialty. While there are more ChatGPT medical applications, their overall design has some restrictions. Sometimes, they cannot access the proper knowledge for their field, manage difficult terms in medicine and find it tough to deal with sensitive data of patients. The Main Differences Between the Two ChatGPT This technology is a general-purpose language model. It can handle different topics in text, though not specifically designed for medical language, procedures, or industry processes. ChatGPT does not meet HIPAA standards on its own. Dealing with patient information in general requires considerable changes, encryption, and updated healthcare privacy technology. Because ChatGPT does not explain its reasoning, it may be difficult to rely on it in making medical decisions. Healthcare Specific AI AI technology used in healthcare is made with medical areas in mind. With the help of medical information and guidelines, models in this field gain accuracy and dependability. The Healthcare-specific AI tools made for healthcare are all created with compliance to both HIPAA and other regulations in the sector. They always ensure that your data is private and secure. Specific AI models for healthcare often help explain the process behind a recommendation or diagnosis. This helps healthcare professionals trust each other and provide treatment based on research. Book Free Demo Use Cases In Medical Software While both types of approaches help, the results can depend on the chosen application. Here, we compare the use of different models in examples: AI Applications in Electronic Health Records: The purpose of using AI for electronic health records (EHR) is to lessen the amount of paperwork and improve the way data is accessed. Models used in healthcare often do data entry tasks, condense doctors’ notes, and discover errors in medical records with more reliability since their data is organized. Enhancing Healthcare with Natural Language Processing: Without NLP, interpreting doctors’ notes, radiology reports, or discharge summaries would not be practical. Although ChatGPT is effective in general NLP in healthcare, healthcare-specific NLP tools are more accurate at identifying elements in medical records and codes. Many times, these tools are included in decision tools and automated checking methods. Supporting Clinicians Through Decision Tools: With clinical decision support AI, physicians use patient information and get guidance based on evidence. An advantage of AI tools for healthcare is that they rely on methods and tools verified in real clinical settings. Forecasting Patient Outcomes: Predictive analytics in healthcare AI to predict a patient’s outcomes, the possible need for readmission, and the future stages of a disease. Custom AI models trained with hospital data are more accurate than others. Improving Telemedicine with AI in Patient Communication: It is becoming increasingly necessary to apply AI for patient communication in telemedicine and after leaving the hospital. ChatGPT can communicate with patients to respond to basic inquiries, remind people of their appointment,s or offer background information. Ensuring Patient Privacy: It is important to use HIPAA compliance and AI to ensure the privacy of patients is protected. The development of healthcare-related AI systems considers compliance issues and includes encryption, access control and audit logs. Automating Administrative Tasks in Healthcare with AI: It is helpful for healthcare to use AI to automate the repetitive duties of making appointments and issuing bills. But when it comes to AI integration in hospital software, using internal systems and rules for each patient, AI in healthcare does the work best. Comparing Medical Chatbots and Custom AI Solutions Unlike custom AI systems, AI chatbots in healthcare are simple to add and can handle a large workload, though they are less knowledgeable about medicine. Although it takes more time to build a custom AI system, the results are more accurate, conform better to rules, and keep patients more involved with their own health information and treatment plans. Role of OpenAI in Advancing Healthcare Technology OpenAI is being incorporated in healthcare by forming partnerships with healthcare technology firms and research teams, including its integration into Clinic Management Software to enhance administrative efficiency and decision-making. At the same time, there are still concerns related to protecting data, ensuring its accuracy, and maintaining regulatory compliance. To effectively use OpenAI in critical medical settings, additional safeguards and system enhancements are necessary. Conclusion Whether to use ChatGPT or a healthcare-specific AI depends on the organization’s plans, the amount of money available, and the rules they have to follow. While ChatGPT is convenient to use and covers many NLP tasks quickly, it may not meet clinical accuracy, compliance, or integration requirements. FAQs [sc_fs_multi_faq headline-0=”h3″ question-0=”Is there a difference between ChatGPT and healthcare-related AI?” answer-0=”While ChatGPT can be used for various applications, healthcare-specific AI is built
7 Ways LIMS Can Automate Your Lab As more laboratories embrace digital technology, automation is now fast becoming an essential building block of laboratory operations. Automation helps keep track of huge volumes of samples, maintain data integrity, remain compliant, and assists in Optimized lab workflows to be highly competitive in scientific research or diagnostic operation. A Laboratory Information Management System (LIMS) provides all the solutions necessary. By implementing a LIMS, laboratories can automate processes, minimize human errors, and enhance productivity in all aspects of work. This article discusses what LIMS automation is all about and delves into seven tremendous ways it can automate and revolutionize your lab. What is LIMS Automation? LIMS automation involves the method of using computerized software functions and tools within a Laboratory Information Management System to carry out routine or intricate operations automatically. To enhance precision, reduce turnaround time, and increase the efficiency of operations in the laboratory. LIMS automation enhances the automation of operations such as data capture, scheduling of tasks, management of workflows, reporting, and complying with regulations to lead to maximized performance of the laboratory. Learn more about LIMS Automation. Significance of Automation in Today’s Laboratories Meeting the Needs of High-Volume Operations: Today’s laboratories need to analyze thousands of samples and produce high volumes of data daily. Manual data entry and documentation just can’t meet this need. Automation allows laboratories to manage higher workloads without sacrificing speed or accuracy. It guarantees results are delivered on time, eliminating backlogs and turnaround times. Improving Accuracy and Data Integrity: Human error is among the major sources of erroneous results in laboratory settings. Automated systems provide uniform performance through reduced human intervention. Whether it is data input, computation, or sample traceability, automation guarantees that each process follows predetermined protocols. Thus, the integrity of better data and reproducible scientific results. Automated Compliance and Reporting: These rigorous regulatory demands upon laboratories, which include comprehensive documentation and traceability, are known. The logs automatically kept by the system provide an accurate record of all actions for audits, minimizing human error to the extent possible, which is vital for inspections and maintaining certifications. Assisting Laboratory Personnel: By means of automation in routine and administrative jobs, laboratory professionals can concentrate on the analytical, research, and strategic aspects of work. This boosts job satisfaction, and it consolidates the lab as an innovational and scientific space. Here are 7 Ways LIMS Can Automate Your Lab 1. Automated Data Capture Manual entry of data is one of the most prone-to-error operations within laboratories. LIMS offers automated capture of data, capturing data directly from devices and instruments. There is no manual transcription, which minimizes the risk of typographical errors or missing information. Such equipment as robotic pipettes, spectrophotometers, and chromatographs can interface with LIMS for accurate and real-time data acquisition. With automation, traceability is facilitated, as well as decision-making time using sound results. 2. Task Scheduling in the Laboratory A well-organized lab operates like a well-oiled machine, and that’s where scheduling tasks in the lab comes into play. LIMS can automatically schedule task assignment by calculating resource availability, prioritizing urgent samples, and assigning staff and equipment usage in an optimal way. For instance, routine quality control tests, instrument calibration, and maintenance schedules can be automated without manual intervention. It ensures that there are no skipped tasks, balanced workloads, and timelines consistently met, increasing overall lab productivity. 3. Effective Lab Workflows Workflows form the foundation of any lab process. LIMS enables labs to achieve effective lab workflows by defining step-by-step processes for different sample types, tests, and quality controls. These workflows are electronic and eliminate vagueness and guarantee consistency for several departments or sites. LIMS incorporates conditional logic, which allows the lab to reroute samples to re-test or further analyze them automatically based on initial results. This structured automation not only makes the lab more efficient but enhances the lab’s scale-up capabilities. 4. Automated Compliance within Laboratories Automated compliance in laboratories with regulatory standards such as ISO, CLIA, and FDA is necessary. Automated laboratory compliance with LIMS ensures that every activity and data point is monitored with appropriate timestamping, user IDs, and version control. Automated audit trails and compliance reporting decrease the administrative workload of laboratory personnel. Automated reminders for calibration, validation, and certification due dates ensure laboratories remain compliant and inspection-ready at all times, therefore eliminating the potential for penalties or shutdowns. 5. Remote Access to Laboratory Management The modern lab environment is usually in the form of remote workers or multi-location facilities, and therefore remote access to lab management becomes increasingly important. A cloud LIMS allows trained staff to access lab data, monitor workflows, and generate reports remotely. This is advantageous when lab managers, researchers, and QA personnel need to manage processes without being physically present. Real-time dashboards with user-specific access control support operational transparency and data safety. 6. Lab Calculations Done Automatically Laboratories typically require lengthy and monotonous mathematical computations for some tests and experiments. Manual computation is time-consuming and error-prone. LIMS provides Automated calculations in labs by combining algorithms and formulae into the system. Reproducibility, accuracy, and speed are provided across analysis by this. In case it’s for the calculation of concentration, dilutions, or rate velocities, computer-assisted computation makes the burden light on the workers in laboratories and ensures reproducible and accurate outcomes. 7. Reporting and Documentation Automation Accurate and timely documentation is the key to lab performance, regulatory compliance, and client communication. Reporting and documentation automation becomes a piece of cake with LIMS. The system is able to generate standard reports, custom formats, data summaries, and trend analysis automatically. Reports can be run at pre-specified intervals or triggered by some events, like completion of a test or approval of a sample. This automation saves time, makes things more transparent, and allows labs to maintain an orderly digital repository of all the important documents. Book Free Demo Facilitating Capabilities for Lab Automation Inventory and Sample Handling: A good LIMS possesses Inventory and sample management modules that monitor
Immunization Tracking through EMR Software Made Easier As healthcare increasingly shifts to digital solutions, Immunization Tracking through EMR software is transforming how we manage and monitor vaccinations. What was once a complex, paper-based process is now a streamlined, efficient system powered by advanced software, giving both practitioners and patients complete control. From flu shots and travel vaccinations to routine pediatric immunizations, EMR systems are essential for ensuring timely doses, minimizing errors, and providing healthcare providers with centralized, easy access to patient records. This is especially valuable in today’s interconnected, networked healthcare landscape. Major Features Of EMR Immunization EMR software provides measurable benefits of much greater value than convenience. Here’s the payoff in its entirety: Real-Time Record Keeping: Eliminates delay and errors associated with manual entry. Reminders and Alerts: Provides automated reminders, reducing the likelihood of dose omissions. Improved Data Sharing: Conveniently shares vaccine history with schools, employers, or other healthcare providers. Compliance Support: Helps clinics meet national vaccination standards and reporting mandates. Time Savings: Freeing up valuable administrative time, enabling providers to devote more time to patient care. All these amount to improved practice, improved patient safety, and improved public health. Application & Benefits Of Immunization Tracking by EMR Software The Value of Accurate Immunization Records Vaccines are a foundation of public health. Vaccines prevent infectious disease spread and save a million lives annually. But vaccines are only effective if there is the schedule and dosing adherence. That is where accurate immunization records come into play. Paper or tainted records, however, have the undesirable consequence of causing missed doses, duplicate injections, and even becoming a health risk. They are misplaced or missing in emergency conditions or patient transfer between providers. These problems are addressed by EMR systems. Monitoring computerized allows all doses administered to be accurately documented, creating an entire lifetime history of immunizations available at any authorized location. Successful Vaccine Management through EMR Systems Core EMR software must have the ability to automate sophisticated clinical workflows. Immunization tracking is now baseline functionality for almost all EMR systems, and this is how it works: If a vaccine is given, it’s entered on the patient’s electronic record. The software captures important information like the type of vaccine, the manufacturer, the lot number, the location where given, and the provider. This information is then stored indefinitely and added to the patient’s entire medical record. Much more importantly, the system tracks follow-up doses and reminds providers and patients of due or past-due immunizations. This automation avoids vaccinating on schedule delays without reminders. Automated Alerts: Provider Safety Net The favorite thing about EMR-based monitoring for immunization is the automated alert. The provider does not have to go on a wild search for patient records to discover upcoming vaccinations. The system uses reason-based scheduling to produce reminders for all patients based on age, medical history, and recommended vaccinations. For example, children are tracked against early child vaccine schedules, and adults are reminded of shingles, pneumonias, or flu vaccines. The predictive alerts prevent failure of vaccination, thus making individuals and populations safe otherwise at risk. Patient Empowerment Through Digital Portals Healthcare today is heading towards the patient-focused direction, and EMRs are at the center of it. By integrating patient portals with EMR systems, now patients can conveniently access from home to see their immunizations, appointment reminders, and even place orders for copies of their records online. This puts patients well-informed and activated. Parents can track vaccination history on children, adults can track booster shots and flu shots, and travelers can track being ready to go at the destination. Second, electronic reminders timed, through SMS, email, or push notification, radically increase rates of compliance. Integration with National and Global Registries Most EMR solutions are also designed to integrate easily into government immunization registries and health information exchanges. This allows clinics to Develop reports needed by national or local health authorities. Use state-wide or nationwide immunization statistics as a reference. Improve disease surveillance and response to outbreaks. The unity strengthens public health infrastructure and facilitates quick response during emergencies like pandemics or disease outbreaks. AI and Predictive Vaccine Management As EMR software matures, artificial intelligence and machine learning are being used to enhance the forecasting of vaccines and activation of patients. For instance, EMRs will be in a position to forecast who will be most likely to miss an upcoming vaccination and automatically schedule follow-ups. They can even use population-level information to inform policymakers where they have to prioritize vaccinations during crisis. This idea of leadership reframes immunization tracking from passive to active, proactive, serving the entire healthcare ecosystem. Best Practices for Optimum EMR Immunization Solutions To aim towards maximum benefits of monitoring immunizations using EMR software, doctors and health practitioners must have the following in place: Train Healthcare Personnel Appropriately: Train all health personnel in recording vaccine information and viewing immunization calendars on the software. Standardize Documentation: Document on the same types of documents across the entire network, avoiding error entries and enhancing the quality of information. Make It Cross-Accessible: Allow sharing immunization records in real-time across departments or even offices within the network of health centers. Audit Records Frequently: Regular audits prevent missed doses, repeated doses, or incorrect recording. Budzing these practices into work on a daily basis, health centers are able to provide more uniform and reliable immunization services. Real-World Impact: Community Health at Scale When EMR immunization software is effectively installed in clinics, schools, pharmacies, and hospitals, the effect quickly scales. Where EMR integration is strong, governments have reported: Improved vaccination coverage Improved speed in ending outbreaks Better vaccine
3 Medical Affairs Trends Impacting the Industry The ideal landscape of medical affairs is being driven by technological innovations, evolution in regulations, and the growing needs of an increasingly demanding patient base pressing for more patient-centeredness into care. The professionalism of medical affairs is called upon by properly ensuring that new scientific knowledge is diffused into practice adequately at the apex of the clinical practice–regulatory–pharmaceutical triad. Being successful in a very dynamic field, it has become very necessary for professionals to stay attuned to changing trends within their respective industries. The article is going to cover current trends incorporated in medical affairs that are useful today and lie at the core of shaping the future concerning healthcare and pharmaceutical innovation. 1- The Rise of Digital Health and Integration of Technology Digital health technologies are innovating the way medical affairs work through new tools and platforms for better communication, data analysis, and decision-making. Not a fleeting trend, technology’s role in medical affairs has been a fundamental shift changing industries. Improved Analytics and Insights: Perhaps the most important influence of digital health on medical affairs is the sophisticated application of data analytics. All these technologies of big data, AI, ML have been used to analyze bundles on healthcare data with their possible insightful results, which otherwise would be hard to get. That puts medical affairs professionals in a position where they have to follow through on trends more closely, prove to be better at prognosis, and allow data-driven decisions to help improve quality in clinical trials, drug development, and patient care. Virtual Engagement and Communication The pandemic has vastly accelerated the transition to virtual engagement tools, and this is unlikely to be reversed. Medical affairs professionals will increasingly look for meeting, conference, and discussion venues with HCPs on virtual platforms. Virtual engagement does have its own advantages, which include easily reaching a global audience, reducing travel costs, and sharing updates in medical information on a timely basis. Virtual advisory boards, webinars, and digital content dissemination are fast becoming business as usual for maintaining strong relationships with key stakeholders while the medical affairs team learns to adapt to new demands brought about in a digital world. This shift will also meet the increasing on-demand requirement for medical information that HCPs express by engaging at their convenience with content. 2- Patient-Centricity and Real-World Evidence A few years ago it was nothing but the buzzword du jour, but now patient-centricity has been taken up by medical affairs teams as a tenet on which to ground their strategy and operations. And the patient is very relevant to the success of new therapies and medical innovations now. Patient Engagement in Research and Development It is one of the biggest trends: patient orientation, which gives even more impetus to increase the involvement of patients in the R&D process. Medical affairs teams work with patients to understand their experience, preferences, and unmet needs. Great importance is placed on the value contributed by patients to the improvement of study designs in regard to clinical trials, the relevant endpoints, and new therapy relevance in the real world. PROs are rapidly becoming an established constituent of clinical trials that tell perception directly by patients about treatment benefits against side effects. This more than slightly raises tennis of certainty that new drugs will not only meet regulatory requirements established by the authorities but also bring meaningful benefits for patients. Book Free Demo Real-World Evidence Real-world evidence and patient-centricity, thus, run hand in hand. Medical affairs teams drive how RWE can complement the use of classical clinical trial data through the provision of a complete picture of the effect a therapy will have on various patient populations. Real-world evidence really comes into its own in the domain of long-term outcomes, rare side effects, and treatment efficacy in standard practice. This further shifts the emphasis to RWE, which has already had a bearing on regulatory decisions recently as agencies like the FDA make more use of RWE in their reviews. What this trend does is to place a critical tag on the securing and analysis of data from real-world sources by medical affairs professionals in the processes of development and approval for new therapies. 3- Evolving Regulatory Landscape and Compliance It is in continuous flux for pharmaceuticals, with new guidelines, policies, and standards continuing to emerge to try to grapple with the complexities in the modern healthcare. Staying current with the evolution of the regulations by Medical Affairs professionals and successfully charting the complexities within the regulatory environment is mandatory to avoid noncompliance. Increased Scrutiny on Data Transparency The data transparency trend continues to be rampant in the broader key trends of the regulatory landscape. Increasingly, this means increasing weight upon disclosures of clinical trial data, adverse event reporting, and real-world evidence by regulators. That is all driven by the need to ensure the public trust, safety of patients, and informed decision-making. Medical affairs teams are keen on ensuring the data are communicated to regulatory bodies, health professionals, and patients in an accurate and transparent way. This, in effect, encompasses more than compliance with the law and actually dissemination of information proactively with the view of supporting safe use and effective treatments. Global Harmonization of Regulations The more globalized the industry becomes, the stronger the push is toward the international harmonization of regional regulatory standards. Organizations like the International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use are trying to harmonize better regional guidance in such a way that it is going to be easier for a company to manage international markets. This requires the medical affairs professional to have in-depth knowledge not only of the global regulatory environment but also of local requirements. A current international guideline to understand, then building collaboration between experts in the fields of medical affairs and regulatory science is very important to compliance and facilitating a global launch of new therapies. Focus on post-marketing surveillance Recently, interest from these areas of post-marketing surveillance by regulatory
Everything You Need To Know About Medication Management Medication management consists of all activities that ensure a patient uses their medication as prescribed to ensure the desired results. Medication management is described as the wide array of activities in relation to the prescription, dispensing, administration and monitoring of medications. This comprehensive guide shall go right into the crucial elements of medication management, benefits, challenges and best practices. What is Medication Management? Medication management is the process of how a patient’s medications are managed; it refers to the process by which it is ensured that the right medicine has reached the patient, that the right dose has been administered, and the medicine is taken in adherence to the schedule and the required therapeutic effect has been derived. This context enjoins the different health professionals at the helm, including the doctors and pharmacists down to the nurses and the patients. Medication Management Elements 1- Medication Reconciliation Medication reconciliation is the process of obtaining accurate list of all the medications that a patient is on. All prescribed medications and all the over-the-counter drugs, herbal supplements, and vitamins should be noted. The concept is to leave no allowance for discrepancies or potential interaction of different medications. 2- Prescribing Prescribing would mean the selection of a drug appropriate for a particular condition of the patient. One requires absolute knowledge regarding the history of the illness, the current health status of the patient, and the drug interaction. Prescribing also involves clear instructions regarding how and when to take the medication. 3- Dispensing Dispensing is the stage at which the medication is prepared with the right formulation and dispensed to the patient. It is of great significance in the role of a pharmacist in ensuring the proper labeling of the medication and how the patient is going to take it. 4- Administration Administration refers to taking or giving a drug as directed. It can be carried out by the patient, carer, or a health professional. The end result of taking or giving a drug is often influenced by how well a drug has been administered. 5- Monitoring It involves monitoring the reaction of the patient to the medication. In some cases, measuring effectiveness and side effects and change of medication if need be. It always includes follow-ups and laboratory tests. Benefits of Medication Management 1- Improved Patient Outcomes Effective medication management helps improved health outcomes and ensures that patients take their medicines as prescribed to reduce complications, readmission into the hospital, and progression of disease. 2- Improved Patient Safety Mismanagement of medications in relation to dosing and drug interactions can even lead to fatal mistakes. Proper management of medications reduces such risks, as it illustrates good general coordination that supports optimal prescribing and good dispensing and administration practices. 3- Saving Costs Correct medication management saves the health system costs by avoiding medication misadventures with their related complications, including lowered rates of hospitalization, emergency room use, and long-term complications that pose more difficulties with one’s health. 4- Patient Empowerment Patients who are informed and involved in their medications are more likely to adhere to the treatment plan. Engaging a patient in care, especially in medication management, gives one an opportunity to take a lead role in matters of health which improves general experiences. Challenges to Medication Management 1- Complexity of Regimen A good number of patients, the majority of whom have chronic conditions, may be under multiple medications. One of the complications that arises when handling such regimens is related to the risks of medication-making errors and non-compliance. 2- Non-Adherence by Patients The most serious pharmacological problem blamed for the integral component is poor adherence to the regimen, leading to unsatisfactory health results. Forgetfulness, misunderstanding the instructions, intolerable side effects, and lack of money are common problems related to non-adherence. 3- Communication Barriers The clear communication between the health care providers, patients, and caregivers among whom medication management should be successful is marred by a few barriers limiting the process according to the effectiveness such as language problems, health literacy issues, and fragmented care. 4- Medication Errors Even with the best effort to prevent it, medication error still occurs. The error may occur in any of the steps involved in the medication management process and may emanate from either human failure or system failure, poor education, or training. Book Free Demo Role of the Pharmacist in Medication Management Pharmacists have a significant role in the process of medication management. Their strong knowledge in regard to drug therapy assures adequate drug dispensing by educating the patients properly regarding use. In relation to medication management, a pharmacist can provide the following significant roles: Perform medication review and reconciliation Monitor for potential drug interaction and side effects Provide MTM services associated with medications Instructing patients and their carers when to use medications as prescribed Array Consult other healthcare teams for relevant management programs Medication Management in Special Populations 1- Elderly Patients Since the elderly are always afflicted with co-morbidities and usually on more than one medication, they are bound to be victims of medication errors and their resultant effects more frequently than others. The basics of medication management in the elderly patient, therefore, would pertain to simplification of the regime, watching out for DDIs, and including the caregiver in the process. 2- Pediatric Patients As children are of smaller stature and their bodies are yet developing, proper dosing and monitoring should be observed. One should provide age-appropriate education with close liaison with the parents or guardians on medication management for the pediatric patients. 3- Chronic Disease Patients The cases that benefited most from more-realized benefits of the practice of medication management include those with chronic illnesses, such as diabetes, hypertension, and asthma. Effective management of conditions like those indicated requires constant monitoring, supplemented by patient education that supports compliance. Future Trends of Medication Management 1- Personalized Medicine Genomic and pharmacogenomic research open up the field to treatment that is personalized based on one’s genetic makeup and thus improves medication efficiency