Low-Code & No-Code in Healthcare: Transforming Digital Innovation Without Heavy Coding The healthcare sector faces fast tech changes, yet standard software methods tend to be sluggish, costly, or rely heavily on scarce IT staff. That’s why low-code healthcare platforms and no-code healthcare solutions are gaining ground in medical settings. Instead of coding from scratch, care centers can now create apps through visual interfaces. Automation becomes easier for routine tasks across clinics and health networks. With these platforms, teams design tools tailored to their needs, even without developer support. In this guide, we’ll look at what these systems are; then examine why healthcare relies on them. Real examples show where they’re used, highlighting advantages alongside obstacles. Finally, discover how such tools influence future advancements in health technology. What Are Low-Code and No-Code? Low-code and no-code platforms are software development tools that allow users to create applications with minimal or no coding. Low-Code Platforms Low-code solutions offer: Drag-and-drop interfaces Pre-built components Adaptation using simple coding These tools work well for creating simple low-code EMR software, hospital systems with minimal coding, low-code clinical software that requires less programming, also digital health products built quickly. No-Code Platforms No-code tools let people create apps through drag-and-drop screens or form creators, using automation features instead of code. These often serve to build: No-code telemedicine platforms No-code patient management tools for handling patients No-code EHR solutions No-code digital health tools for digital health Each method lets medical groups build systems more quickly while cutting costs compared to standard methods. Why Healthcare Needs Low-Code and No-Code Solutions? Healthcare faces distinct issues like strict rules, not enough workers, complicated processes, also ever-increasing patient information. Low-code and no-code tools solve these pain points by enabling: 1. Faster Digital Transformation Hospitals can skip long waits for software. Because of fast development, medical apps are built quickly through rapid healthcare app development. Teams now release tools in days, sometimes just a few weeks. 2. Reduced IT Burden Some medical centers don’t have big tech groups. Still, these systems let nurses and office workers create what’s necessary, without coding skills. 3. Affordable Technology Expansion Classic bespoke software comes at a high price. Meanwhile, low-code or no-code options cut expenses by around 60% to 80%. 4. Improved Workflow Efficiency Several medical centers continue using handwritten records. Yet digital health automation streamlines operations, cutting mistakes while boosting efficiency. 5. Better Patient Care Digital health tools help doctors save time, so diagnoses happen quicker; this boosts teamwork among staff while patients get healthier results. Healthcare needs better tech that adapts quickly, so low-code or no-code tools are now essential rather than optional. Book Your Free Marketing Consultation Key Use Cases in Healthcare Low-code or no-code tools open many practical options. Among the strongest examples are: 1. Electronic Medical Records (EMR) & Electronic Health Records (EHR) Hospitals may develop custom low-code EMR tools, while also designing no-code EHR systems that match their processes. 2. Telemedicine Applications Clinics might build no-code telehealth tools fast, using them for virtual visits, web-based booking, or e-prescriptions. 3. Patient Management Systems Create simple digital tools without coding: Manage appointments through automated reminders Use dashboards to handle check-ins instead of manual logs Streamline payments via integrated invoicing systems Enable messaging features for smoother conversations between visits 4. Hospital Management Tools Low-code hospital management system simplifies creating hospital tools for admissions, also streamlining how staff are assigned. It supports pharmacy monitoring while improving control over supplies. Systems become quicker to deploy due to reduced coding needs. Each function integrates smoothly without complex programming. 5. Clinical Decision Support Tools Using simple coding tools, healthcare groups build logic-driven apps that help physicians decide on diagnoses or therapies. These systems guide medical choices via automated rules instead of complex programming. 6. Digital Health Automation Healthcare workflow automation includes: Lab reporting workflows might use digital tools to run automatically Insurance claim steps could operate via tech solutions Triage setups may function through system automation Discharge summary tasks can work using smart software 7. Custom Mobile Apps Groups may create phone tools for nurse checks through healthcare app development, handling equipment, gathering patient opinions, or sharing messages inside departments. 8. Data Dashboards & Analytics Low-code platforms can integrate real-time data to provide dashboards for hospital administrators. These examples reveal how simple and strong low-code or no-code platforms are within today’s medical setups. Benefits for Healthcare Organisations Adopting low-code and no-code tools offers major advantages: 1. Speed Companies may develop software ten times quicker by leveraging fast medical application builders. 2. Lower Cost Less demand for big coding groups or costly tailored programs. 3. Customization Hospitals may adapt tools to fit how they work rather than reshaping routines around programs. 4. Empowered Staff Non-tech team members are able to build digital health solutions addressing actual needs, using simple methods or practical approaches, to reach meaningful outcomes. 5. Easy Integration Many platforms work well with current health tools, such as EMRs or labs, and also connect to hospital records. While some link directly, others need minor adjustments; each setup varies by site. Compatibility depends on structure, yet most adapt without major changes. 6. Better Patient Experience Faster service comes through automation; better care follows clearer communication. 7. Scalability Applications scale smoothly when businesses expand, while updates roll out without hassle. Challenges & Considerations of Low-Code and No-Code Though strong, these tools bring difficulties too, yet they’re useful despite drawbacks. However, issues arise alongside benefits; still, people keep using them regardless. 1. Data Security and Privacy Medical services deal with private details. Firms need to confirm systems meet HIPAA rules, follow GDPR standards, or adhere to regional laws. 2. Limited Customization in No-Code No-code solutions might limit advanced app features. 3. Vendor Lock-In Some platforms limit moving data or apps to different systems, migration becomes a challenge due to restrictions built into the design. 4. Need for Basic Training Although programming isn’t necessary, employees must learn how to build smooth processes, through proper instruction. Yet without hands-on practice, workflow planning may
The Future of API Integrations in Healthcare Technology is changing the landscape of health. In technological advancement today, API integration of EHR systems is cited as the most important and the biggest impact of technological advancement in creating new chances for delivering quality care and improving operations as well as service provision. APIs are application programming interfaces that connect various healthcare systems for easy communication among hospitals, clinics, pharmacies, and laboratories, and payers, making it simple for all of them to share data. Unison of communication extends from the interfacing across the different platforms, allowing healthcare professionals to access all patient information in real-time, which is likely to affect developing better-informed and better quality services. As healthcare data evolves, and becomes increasingly complex, the demand for Health tech APIs, which can manage and work with high volumes of patient data, is exploding. Specifically, FHIR healthcare APIs have arisen as a strong tool for making this process easier. FHIR ensures the easy sharing of all kinds of medical data between different healthcare systems by promulgating standardized formats of sharing medical data interchange. Understand the Current Landscape of API Usage in Healthcare APIs or application programming interfaces are the things which connect different software applications, which allows good communication and exchange of the data between those applications or pieces of software. APIs for health care allow different systems like electronic health records and lab information systems to connect to billing systems more easily, even with health systems in insurance. One of the most promising developments is the FHIR Healthcare API trends (Fast Healthcare Interoperability Resources), which are helping in the standardization of data formats and Interoperability in healthcare. FHIR is a health information exchange (HIE) framework designed to facilitate data exchange and understanding from system to system under the auspices of HL7. Furthermore, integration of third-party health applications has expanded the scope of healthcare systems and is considered to uplift patient engagement and personalized care. When incorporated through APIs, these apps can access and add to patient records and are capable of scheduling appointments, sending medication reminders, and tracking health. Some Benefits of API Integrations in Healthcare The optimization of healthcare systems through integrating APIs into them brings a multitude of benefits: Enhanced Data Exchange: APIs allow patient information to be shared in real time over several different healthcare platforms, thus allowing better coordination between the providers. This results in better and more timely decisions, hence, delay in care is reduced and better care outcomes are achieved. By making sure that all the healthcare workers involved will have the same current information at their disposal, API integration reduces the chances of misunderstanding. Improved Patient Engagement: Through patient data APIs, it is possible for a patient to get hold of health records, lab test results, prescriptions, and their treatment plans with ease. This flexibility allows patients to become agents in their health management and establish a partnership with their medical caregivers. It encourages them to stick more closely to treatment plans and has better long-term health outcomes. Operational Efficiency: By automating administrative procedures, e.g., appointment scheduling, verification of insurance, and handling the billing cycle, the burden of manual workload is reduced on healthcare staff. Not only does this reduce people’s errors, but it also increases the rate at which administrative procedures are carried out, subsequently, the healthcare organizations will spend fewer resources and can concentrate more on looking after patients. Innovation and Flexibility: APIs set the infrastructure on which continuous innovation in healthcare is based. They enable Healthcare organizations to rapidly develop and incorporate new applications/services which would respond to the emergent needs. Whether it’s a telemedicine platform or a new mobile health application, or an AI-enabled diagnostic equipment, APIs provide the ability to change according to the changing dynamics of the industry. Secure Data Handling: The patient-sensitive nature of healthcare data calls for strong protocols for the security of patient privacy. The use of secure API healthcare techniques would allow healthcare entities to guarantee that data is encrypted and safely transmitted according to industry standards such as HIPAA. This is useful in protecting the patient information from cyber-attacks, building a relationship of trust between the patient and his/her healthcare provider, as well as adherence to legal and regulatory requirements. Adding these benefits results in more productive healthcare operations and higher satisfaction ratings for the patient, along with easier application of innovative solutions aimed at addressing the ever-changing needs of the sector. Book Free Demo Emerging Trends Of API Integration in Healthcare Shaping the Future Multiple tendencies are forming the future of API integrations in healthcare: Real-Time Data Access: The escalating demand for real-time healthcare data enables providers to make quick, knowledge-based inferences in case of emergencies or normal care, thus enhancing patient outcomes. Personalized Medicine: Now, APIs are facilitating the integration of genomics data, biometric readings, and history of a patient to form highly customized treatment plans with advances in personalized medicine. Telehealth Expansion: With increased mainstreaming of telemedicine, APIs become important to link everything, make the EMR API integration smooth, and ensure data sharing is secure between doctors and patients. This continuity of care improves accessibility of care, especially for remote populations. Integration with Wearables: As smartwatches and fitness trackers become popular, health data exchange APIs are now capturing real-time information such as heart rate, sleep patterns, and activity levels, providing a wider perspective into patients’ health. Artificial Intelligence and Machine Learning: APIs are making AI-powered tools be integrated into the healthcare system. This integration boosts the quality of predictive analytics, helps in early diagnosis, and also boosts the support of clinical decision-making. Systems can provide more accurate evaluations and tailored treatment suggestions by interfacing with algorithms in the form of APIs. Challenges Ahead Related to API Integration in Healthcare However, several obstacles keep APIs from being well-integrated in healthcare systems: Data Standardization: It is still a major barrier to getting uniform data formats on different systems, which affects the efficiency of the health
Why Most Clinics in Pakistan Fail to Scale — And How Software Solves It? The rapidly evolving healthcare industry of Pakistan depends heavily on clinics and small medical practices, which provide essential medical care to numerous patients throughout urban and rural areas. These medical facilities treat patients across millions of individuals throughout cities as well as remote areas. Despite performing critical functions, most clinics in Pakistan encounter difficulties expanding their operations past one clinic or doctor location. The expansion of clinics into multi-location healthcare groups remains rare even within densely inhabited areas. Many clinics in Pakistan face growth limitations which leads to a fundamental inquiry about the causes and solutions for this situation. The solution requires an integration of structural problems with business process weaknesses, coupled with weak digital capabilities as the primary reason for growth stagnation. The implementation of digital health record systems and solutions, combined with clinic management software systems, begins to eliminate the barriers that hinder clinic expansion and sustainable scalability. Understanding The Scaling Problem in Pakistani Clinics The objective of scaling a private clinic business exceeds merely extending patient volume across multiple branches. The goal is to develop standardized systems that provide uniform patient care throughout every operational contact point. The majority of clinics in Pakistan battle organizational excellence because of multiple essential factors, and require the best clinic management system in Pakistan 1. Manual Record Keeping and Data Loss Reliable patient documentation records persist on paper at most clinics that operate in the small to mid-sized category. The lack of proper data management produces various problems, which include lost patient history records along with difficult follow-up procedures and increased chances of data loss. Financial expansion through patient data management proves impossible when retrieval capabilities cannot ensure clinical data accessibility. 2. Lack of Operational Visibility The majority of Pakistani clinic owners together with their medical staff operate their clinics without knowing their operational efficiencies. Clinics are effectively making use of the available appointment times. The medical staff manages to follow their scheduled work protocols. What amount of income does the clinic lose through patients who fail to show up and through incorrect inventory management? These important questions remain unanswered because clinics have insufficient monitoring systems. A data-driven strategy is essential for making strategic expansion decisions since the absence of insights will turn important decisions into mere speculation. New clinic branches reflect identical inefficient operational methods from existing facilities, which produce failure instead of growth. 3. Staff Dependency and Lack of Standardization Multiple clinics in Pakistan rely heavily on selected personnel who grasp their operational systems because only these workers enable proper performance. When essential staff members exit, the system fails to function properly. The facilities lack standard operating procedures (SOPs) to train staff and manage flow operations while processing payments. Business expansion depends on standardized operating systems that serve the company beyond individual employees. The absence of automation and enforcement software preserves the fragile and inconsistent operational status of clinics. 4. Financial Leakage and Untracked Expenses Examining monetary movements remains a significant obstacle for businesses trying to expand their medical operations. Several clinics fail to establish proper systems that track both income and expenses, discounts and patient refunds. Petty cash goes unrecorded. Patient payments might be under-reported. The inability to track financial data undermines any possibility of comprehending whether a clinic makes enough profit to grow. The lack of software-backed patient tracking systems results in conflicts about revenue sharing among doctors who share revenue at multi-practitioner clinics. Book Free Demo How Smart Clinic Management Software Solves These Problems? Digital transformation functions across all healthcare institutions, starting from large hospitals to small clinics. A patient management software platform transforms all medical facilities, even in small clinics, through automated operations and improved patient care and data analytics. Here’s how: 1. Automated Appointment Management When patients use clinic software, they can make appointments using a computer or a mobile device options which cuts both telephone congestion and human mistake rates. Software management tools help doctors schedule appointments better so patients obtain their appointments on time, which decreases missed appointments. Real-time updates maintain constant alignment between clinic personnel as well as medical staff. 2. Electronic Medical Records (EMRs) The EMR software for clinics functionality enables clinics to maintain safe storage of patient information including medical records, laboratory reports and clinical prescriptions. The health care quality measures enhance as the system allows patients to keep their medical history accessible across different network doctors or clinics. 3. Centralized Billing and Payments The central billing feature of clinic management software joins all financial operations, including payments and receipt handling together. The software system provides instantaneous transaction recording and report production, and minimises financial loss through cash theft. Seamless payment processing occurs when certain platforms link with POS equipment and digital payment solutions. Benefits of Centralised Billing: Eliminates manual errors Enables transparent revenue-sharing between doctors The software system allows clinic owners to determine their revenue numbers according to service type and department. Patients have better trust in billing processes because items appear separated in statements. 4. Inventory and Pharmacy Management Clinic automation solutions enable clinics with in-house pharmacies to track supply quantities and expiration dates as well as automatically request reorders for consumable materials. The system prevents unnecessary stocking while ensuring essential drugs, together with consumables, remain available during needed. Advantages of inventory automation: Avoids medicine shortages By implementing this measure, expired products cannot reach the market for sale Reduces theft or unaccounted losses The system generates up-to-the-minute evaluations of clinic stock 5. Multi-Branch Management Through software for multi-branch clinics, users can visualise and control various locations through a unified dashboard. Clinic owners gain centralised oversight of all locations’ activities, which include an appointment system along with revenue generation and employee performance tracking, even when they are not physically present. Courting expansion becomes possible for clinics since they gain direct oversight and control across all their new locations. Conclusion Modern medical facilities that will prosper within Pakistan’s changing healthcare environment must begin their
Immunization Tracking through EMR Software Made Easier As healthcare increasingly shifts to digital solutions, Immunization Tracking through EMR software is transforming how we manage and monitor vaccinations. What was once a complex, paper-based process is now a streamlined, efficient system powered by advanced software, giving both practitioners and patients complete control. From flu shots and travel vaccinations to routine pediatric immunizations, EMR systems are essential for ensuring timely doses, minimizing errors, and providing healthcare providers with centralized, easy access to patient records. This is especially valuable in today’s interconnected, networked healthcare landscape. Major Features Of EMR Immunization EMR software provides measurable benefits of much greater value than convenience. Here’s the payoff in its entirety: Real-Time Record Keeping: Eliminates delay and errors associated with manual entry. Reminders and Alerts: Provides automated reminders, reducing the likelihood of dose omissions. Improved Data Sharing: Conveniently shares vaccine history with schools, employers, or other healthcare providers. Compliance Support: Helps clinics meet national vaccination standards and reporting mandates. Time Savings: Freeing up valuable administrative time, enabling providers to devote more time to patient care. All these amount to improved practice, improved patient safety, and improved public health. Application & Benefits Of Immunization Tracking by EMR Software The Value of Accurate Immunization Records Vaccines are a foundation of public health. Vaccines prevent infectious disease spread and save a million lives annually. But vaccines are only effective if there is the schedule and dosing adherence. That is where accurate immunization records come into play. Paper or tainted records, however, have the undesirable consequence of causing missed doses, duplicate injections, and even becoming a health risk. They are misplaced or missing in emergency conditions or patient transfer between providers. These problems are addressed by EMR systems. Monitoring computerized allows all doses administered to be accurately documented, creating an entire lifetime history of immunizations available at any authorized location. Successful Vaccine Management through EMR Systems Core EMR software must have the ability to automate sophisticated clinical workflows. Immunization tracking is now baseline functionality for almost all EMR systems, and this is how it works: If a vaccine is given, it’s entered on the patient’s electronic record. The software captures important information like the type of vaccine, the manufacturer, the lot number, the location where given, and the provider. This information is then stored indefinitely and added to the patient’s entire medical record. Much more importantly, the system tracks follow-up doses and reminds providers and patients of due or past-due immunizations. This automation avoids vaccinating on schedule delays without reminders. Automated Alerts: Provider Safety Net The favorite thing about EMR-based monitoring for immunization is the automated alert. The provider does not have to go on a wild search for patient records to discover upcoming vaccinations. The system uses reason-based scheduling to produce reminders for all patients based on age, medical history, and recommended vaccinations. For example, children are tracked against early child vaccine schedules, and adults are reminded of shingles, pneumonias, or flu vaccines. The predictive alerts prevent failure of vaccination, thus making individuals and populations safe otherwise at risk. Patient Empowerment Through Digital Portals Healthcare today is heading towards the patient-focused direction, and EMRs are at the center of it. By integrating patient portals with EMR systems, now patients can conveniently access from home to see their immunizations, appointment reminders, and even place orders for copies of their records online. This puts patients well-informed and activated. Parents can track vaccination history on children, adults can track booster shots and flu shots, and travelers can track being ready to go at the destination. Second, electronic reminders timed, through SMS, email, or push notification, radically increase rates of compliance. Integration with National and Global Registries Most EMR solutions are also designed to integrate easily into government immunization registries and health information exchanges. This allows clinics to Develop reports needed by national or local health authorities. Use state-wide or nationwide immunization statistics as a reference. Improve disease surveillance and response to outbreaks. The unity strengthens public health infrastructure and facilitates quick response during emergencies like pandemics or disease outbreaks. AI and Predictive Vaccine Management As EMR software matures, artificial intelligence and machine learning are being used to enhance the forecasting of vaccines and activation of patients. For instance, EMRs will be in a position to forecast who will be most likely to miss an upcoming vaccination and automatically schedule follow-ups. They can even use population-level information to inform policymakers where they have to prioritize vaccinations during crisis. This idea of leadership reframes immunization tracking from passive to active, proactive, serving the entire healthcare ecosystem. Best Practices for Optimum EMR Immunization Solutions To aim towards maximum benefits of monitoring immunizations using EMR software, doctors and health practitioners must have the following in place: Train Healthcare Personnel Appropriately: Train all health personnel in recording vaccine information and viewing immunization calendars on the software. Standardize Documentation: Document on the same types of documents across the entire network, avoiding error entries and enhancing the quality of information. Make It Cross-Accessible: Allow sharing immunization records in real-time across departments or even offices within the network of health centers. Audit Records Frequently: Regular audits prevent missed doses, repeated doses, or incorrect recording. Budzing these practices into work on a daily basis, health centers are able to provide more uniform and reliable immunization services. Real-World Impact: Community Health at Scale When EMR immunization software is effectively installed in clinics, schools, pharmacies, and hospitals, the effect quickly scales. Where EMR integration is strong, governments have reported: Improved vaccination coverage Improved speed in ending outbreaks Better vaccine
Top Digital Health Company in Asia by CXO Global Forum InstaCare is proud to announce that the CXO Global Forum has honored it with the prestigious ‘Top Entrepreneur Award’. This recognition reinforces InstaCare’s position as the Top Digital Health Company in Asia and a pioneer in revolutionizing the healthcare landscape. Our innovative solutions and unwavering commitment to healthcare excellence have also earned it multiple accolades, including: Top Digital Health Company in Pakistan Best Healthtech Startup in Pakistan Best EMR and Practice Management Company in Asia These achievements reflect InstaCare’s dedication to leveraging technology to enhance healthcare accessibility, efficiency, and outcomes across the region. Bilal Amjad Reflects on InstaCare’s Commitment “This award is a testament to our mission of transforming healthcare through advanced digital solutions,” said Bilal Amjad, CEO of InstaCare. “We are committed to empowering healthcare providers and patients with tools that elevate care delivery and contribute to a healthier future for everyone.” As a leading digital health platform, we continue to innovate and deliver impactful solutions, including: Electronic Medical Records (EMR) Practice Management Systems Telemedicine Patient Engagement Tools Our efforts are bridging the gap between patients and healthcare providers, ensuring that healthcare is more accessible, efficient, and affordable across Pakistan and beyond. The recognition by CXO Global Forum underscores InstaCare’s vision of setting new benchmarks for healthcare technology, bringing innovation, and making a lasting impact on the healthcare industry.
The InstaCare product team is excited to announce the latest updates in InstaCare Smart Clinic software. These updates offer visibility on new features, improvements, bug fixes, and upcoming features of InstaCare Smart Clinic software. New & Improved Features of InstaCare Smart Clinic Software Improved Urdu translation added in the Prescription module for printing Update in Task Get Bill Detail List List of doctors shown as per the location of the logged in user Super Admin Portal improved with more access permissions added Bug Fixes Minor and Major bug fixes Resolved an issue with MR number duplication Resolved an issue with Date field showing wrong date while editing data in Dental Treatment Plan Resolved an issue with the unpaid amount after calculating the discount amount Resolved an issue with EMR Prescription Medicine Searching Expected Features & Improvements of InstaCare Smart Clinic Software in the next update Dialysis Module Smart Pharmacy Module Modern Appointments Module Laboratory Module Meet & Greet & Have a Cup of Coffee If you want to have a cup of coffee with our team, schedule a visit with us at InstaCare Head Office in Lahore, Pakistan.
The InstaCare product team is excited to announce the latest updates in InstaCare Smart Clinic software. These updates offer visibility on new features, improvements, bug fixes, and upcoming features of InstaCare Smart Clinic software. New & Improved Features of InstaCare Smart Clinic Software New Search feature – Now user can search Patient on Smart Clinic App New Patient List available (for use on Prescription and Bill Creation time) for Smart Clinic App Updated Paged Master Patient List Add reference number in patient list Master account for multiple location users User management module Billing module Appointment reports module Location management module Financial reports module Bug Fixes Minor and Major bug fixes Resolved an issue with Appointment List Resolved an issue with General nutrition prescription prescribed time Resolved an issue with Wrong Time slot intervals in Manager account Resolved an issue with EMR Dashboard links which were not working Resolved an issue with Prescription Pharmapedia which were not working Resolved an issue with Reports module in which Amount Receivable Report was not loading Resolved an issue with Smart Clinic App not having Login Response Resolved an issue with Appointment List which was showing all the appointments and not only the Doctor’s appointments Expected Features & Improvements of InstaCare Smart Clinic Software in the next update Dialysis Module Smart Pharmacy Module Modern Appointments Module Laboratory Module Meet & Greet & Have a Cup of Coffee If you want to have a cup of coffee with our team, schedule a visit with us at InstaCare Head Office in Lahore, Pakistan.
5 Strategies to Increase Clinic Profits without Sacrificing Quality Care Making a profit in the healthcare industry isn’t easy, especially with mounting regulations and ever-increasing expenses. As a clinic manager or business owner, you must stay competitive to ensure your financial stability – but quality patient care should always be top priority. Fortunately, there are ways to increase clinic profits without sacrificing excellence in treatment and services. With these five strategies, you can create an effective plan for both short-term success and long-term growth while maintaining great care for your patients. Keep reading to get started today! Improve patient retention As healthcare providers, we understand the importance of patient retention. When patients feel satisfied and valued, they are more likely to stick with our practices for the long haul. One effective way to improve patient retention is through communication. Taking the time to listen to our patients and address their concerns can go a long way in building trust and loyalty. It’s also important to keep patients informed about their health, treatment options, and any changes to their care plan. Providing personalized and compassionate care is key in making patients feel valued, which in turn can lead to higher patient retention rates. By focusing on communication and personalized care, we can create a positive and lasting impact on the health and well-being of our patients. Optimize scheduling and resource utilization Optimizing scheduling and resource utilization is essential for the success of any business. In today’s fast-paced world, it is more critical than ever to make the most efficient use of resources and time. By analyzing your scheduling practices and evaluating how you use your resources, you can reduce costs, increase productivity, and improve customer service. Scheduling should be done based on customer demand, and resources must be allocated effectively to ensure maximum utilization. Implementing technology such as automation and machine learning can help streamline complex scheduling tasks and improve resource allocation. Optimizing your scheduling and resource utilization allows you to adapt to changing business conditions and stay ahead of the competition. Book Free Demo Utilize technology use EHR,EMR to increase clinic profits The electronic health record (EHR) and electronic medical record (EMR) have revolutionized the way healthcare providers document and share patient information. With the use of these technological tools, healthcare professionals are able to quickly and accurately access a patient’s medical history, allergies, medications, lab results, and more. This ensures that patients receive the highest quality of care possible, as providers have all the necessary information they need to make informed decisions about diagnosis and treatment. Not only does the EHR/EMR improve patient care, but it can also save time and increase efficiency for healthcare providers. Overall, utilizing technology such as the EHR/EMR is a crucial component in the evolving landscape of healthcare. Identify and implement strategies to reduce operational costs while still offering quality care Reducing operational costs while maintaining quality care is vital to the success of any organization can increase clinic profits. One strategy is to streamline processes to eliminate waste and redundancy. This involves carefully analyzing every department’s operations, identifying areas of inefficiency, and developing and implementing a plan to streamline processes and reduce costs. Another strategy is to negotiate with suppliers to ensure that the organization is getting the best prices for goods and services. This may involve forming partnerships with specific vendors and leveraging purchasing power to negotiate better pricing. A third strategy is to invest in technology that can automate certain processes, reduce manual labor, and provide useful data insights for continued improvement. Implementing these strategies can help organizations save money without sacrificing quality care for their patients. View More: How Hospital Management Systems are Revolutionizing Healthcare Develop a comprehensive patient care plan to increase clinic profits Developing a comprehensive patient care plan is essential for improving the overall quality of health care and to increase clinic profits. It involves creating a personalized plan that outlines the patient’s medical needs, treatment goals, and expected outcomes. To develop such a plan, healthcare providers need to consider various factors such as the patient’s medical history, current health status, lifestyle, and preferences. They should use evidence-based practices and involve the patient and their family members in the decision-making process. The plan should also be regularly evaluated and updated to ensure it is meeting the patient’s needs. A well-designed patient care plan can improve communication between healthcare providers and patients, increase patient satisfaction, and ultimately lead to better health outcomes. Conclusion The truth is, there’s no one size fits all approach to increase profits and maintain high-quality care. Finding a balance between the two can be an uphill climb, and it’s important to keep trying different strategies until you find one that works best for your clinic. In any case, these five strategies can provide an effective and meaningful starting point on your path to healthier financials without compromising quality care. So don t be afraid to get creative! Evaluate what matters most to your clinic, craft a plan of attack, and give yourself the edge needed for success. Your chances of success will exponentially increase if you implement a combination of these five strategies with determination and consistency. Are you ready to take your clinic from good to great?
What is Best Medical Software For Doctors In Pakistan? In recent years, medical software has established itself as a standard in the healthcare sector. When it comes to best medical software for doctors, there are many different alternatives as well as tools and functions, including EMR/EHR, practice management, medical billing, and patient scheduling. Small specialized clinics, major hospital systems, and other healthcare institutions can all profit from these medical qualities in various ways. Medical software for doctors is becoming increasingly popular, and healthcare facilities have seen increased daily traffic and total sales. Additionally, by deploying specific software systems, health institutions might qualify for government incentives. Involves Key Specifications Knowing the essential components of the best medical software for doctors will also help you to develop a detailed list of specifications for your healthcare facility. This article will also tell you everything you must need to know about the best medical software for doctors in Pakistan. Regular Operations By using medical software, practitioners can spend more time providing treatment for patients and less time recording patient data. The best medical software for doctors can handle many day-to-day activities at your clinic, including scheduling patient visits and controlling your institution’s equipment. Medical software has allowed healthcare organizations of all sizes and types to boost revenue without sacrificing high patient care and service standards. EMR software and other healthcare solutions were initially developed to record patient data electronically rather than by hand. As a result, there were significantly fewer mistakes and improved customer service and healthcare quality. Smart Planning Appointment management software is employed to handle appointments successfully Dynamic scheduling is a common feature of medical software suppliers. This implies that your software could correctly assign specialty equipment to the appropriate exam room and doctor and schedule appointments. Patient Background How long does it take your clinic to research a patient’s medical history? With medical software for doctors, doctors may easily access and edit a patient’s file while archiving and keeping the information for later use. Efficiency And Productivity How long does it also take your doctors to record and locate patient data? Are you treating the most significant number of patients possible each day? Medical software allows doctors to spend more time interacting with the required patients and less time charting or researching patient information. Eliminate Mistakes How frequently do problems with handwriting or legibility cause errors? Most human errors are eliminated when data is entered electronically rather than manually, boosting information accuracy. Medical software may manage every facet of your healthcare organization, from scheduling employees to treating patients. The capabilities needed will change between various healthcare facilities because many different types of medical software are available. Safety And Assistance The confidentiality of sensitive data is one of the most significant benefits of medical software. Many healthcare companies reserved entire rooms to store paper medical records before EHR software was available; these records were considerably more prone to damage, theft, accidental loss, and manipulation. Many medical software suppliers offer training and support films for their users, and some may even assist with the setup and production stages. Most medical software programs provide help by email, phone, or website. Finally Best medical software for doctors and healthcare, in general, has seen significant development. Those healthcare organizations that still need to adopt medical software are merely lagging. Many of these medical software solutions have advantages for patients, your healthcare facility, and staff. Increasing patient participation and interaction improves the patient experience. It’s a win-win situation when you add this to the reality that medical software enables more precise therapy and diagnosis. InstaCare is a group of eminent medical experts providing the best medical software. You can visit instacare.com.pk for further details.
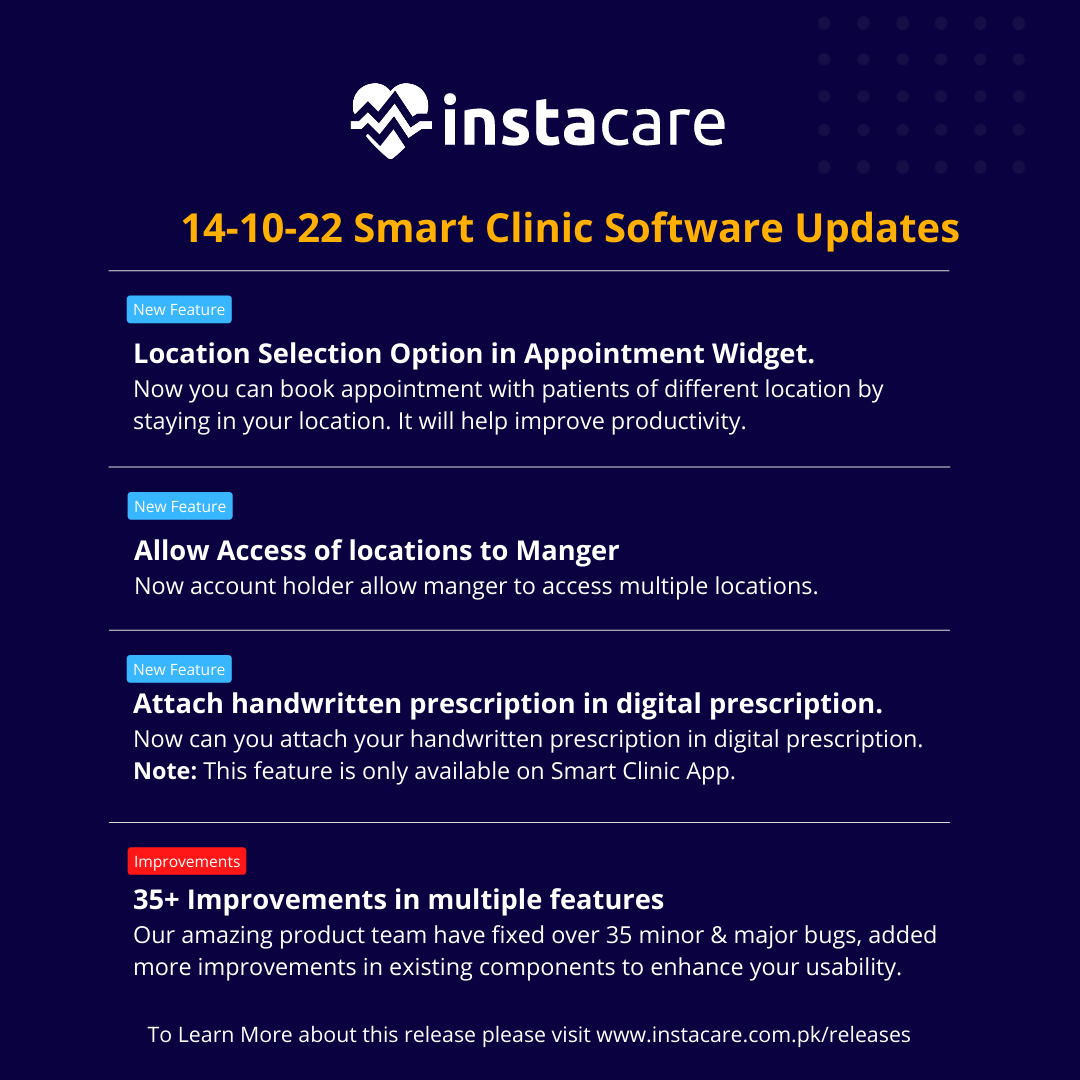
The InstaCare product team is excited to announce the latest updates in InstaCare smart clinic software. These updates offer visibility on new features, improvements, bug fixes, and upcoming features of InstaCare Smart Clinic. New & Improved Features of InstaCare Smart Clinic CNIC selection option on all print pages. Multiple location option on appointment widget. User could search main menus and sub menus. Option to allow access of location to manager. Option to send prescription instructions through voice note. Only available in mobile app. Option to create prescription from Image. Only available in mobile app. Bug Fixes In Appointment booking, users can book an appointment even the slot is booked. In appointment booking showing slots in which doctor not available. Not showing data from 2 to 7 September in appointment calendar view. First time doctor of selected location not showing and appointment can be booked with the doctor who is not available in that location. In Allocation Type, select ward and Room Type dropdown is not in working. In appointment calendar, user’s name is not showing. Start and End time of appointment should show in appointment details. Prevent user to book an appointment with another location user. In multiple location if user reschedule appointment than having no dates. Uploaded file is not showing while editing user details. From web patient book an online consultation but in EMR it’s showing regular checkup. By booking service base appointment duration not showing like in manager account showing. In Eyeglass prescription, not allowing to print prescription. In Eyeglass Prescription not edit prescription also not giving option to update. After logout, system showing 500 error. In billing, patient name not showing by clicking make bill in prescription. In Appointment, Firefox browser not able to select year. User not able to save treatment plan. Enable Urdu to book appointment. User account details not getting update if users do change without uploading any file. Expected Features & Improvements of InstaCare Smart Clinic in the next update Start and end time of appointment in logs. Treatment plan not working in B2B accounts. Treatment Plan when you create treatment by adding new patient, it’s showing the wrong message. Services not showing in Treatment Plan but while printing services are visible. User do not have edited and update option in Treatment Plan. In Telemedicine, if the patient or doctor ends the session, he has to be navigated towards the back screen and should receive a successful session end acknowledgement. User not receiving video consultation link through message. In Telemedicine file updated by patient side, not showing on doctor side. In User & Roles, time slot of appointment not save in set timetable. Screen sharing feature not working properly in online consultation. In Treatment Plan Save button not clickable, automatically saved prescription. Suggest a new feature or report a bug If you wish to suggest a new feature, view the upcoming features, or report a bug, or feel free to write us at success@instacare.software. If you want to have a cup of coffee with our team, schedule a visit with us at InstaCare Head Office in Lahore, Pakistan.
- 1
- 2